Blocking Calcium Ions to Mitochondria Can Kill Cancer Cells Offering a Potential Target for New Drugs
The study, “Selective Vulnerability of Cancer Cells by Inhibition of Ca2+ Transfer from Endoplasmic Reticulum to Mitochondria,” was published in the journal Cell Reports.
This discovery suggests a potential target for new cancer therapies, according to scientists.
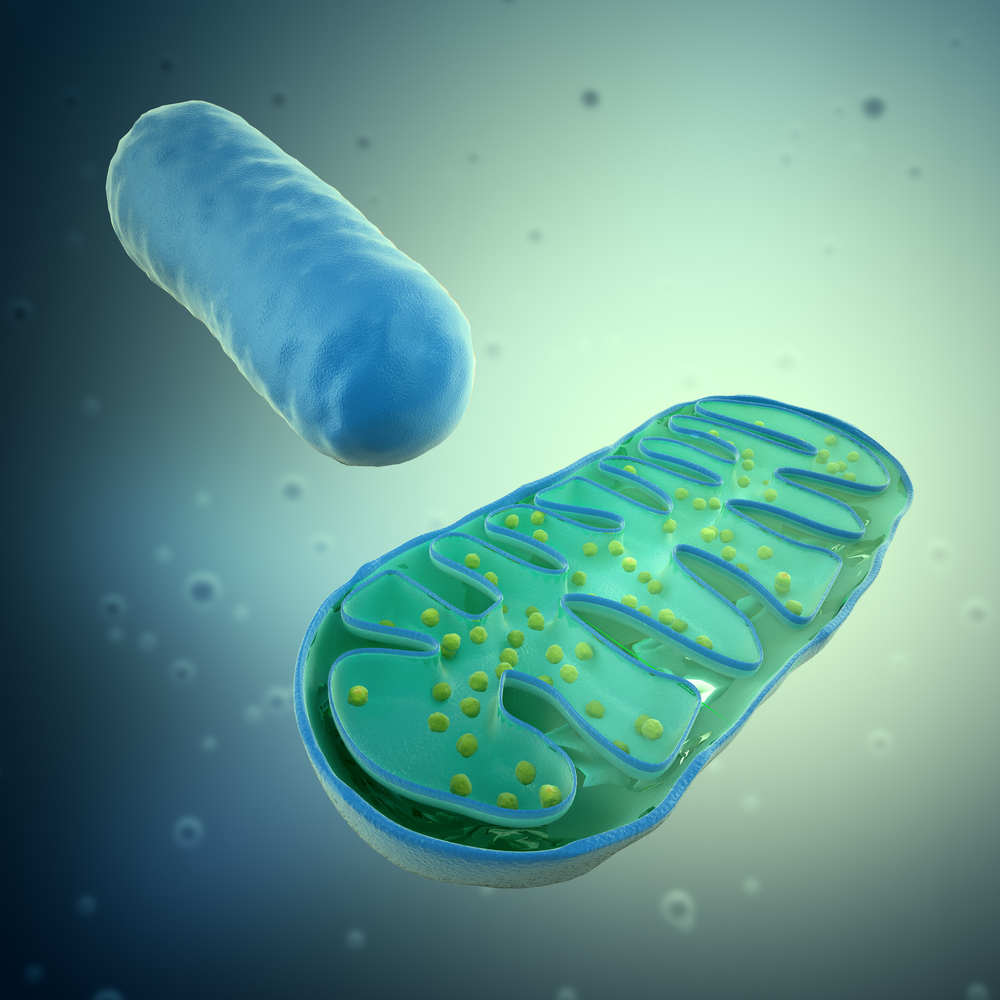
In a previous report, the research team showed that the ongoing shuttling of calcium ions to the mitochondria from another cell organelle, the endoplasmic reticulum, through calcium ion channels called IP3Rs is important for maintaining cell levels of adenosine triphosphate (ATP), a key factor that transports chemical energy within cells for metabolism.
When this calcium transportation is disrupted, they showed ATP levels fall and the cell activates a process of self-eating (autophagy) to survive. This, in turn, induced a bioenergetic crisis in cells leading them to reprogram their metabolism, a phenomenon cancer cells must undergo even in the presence of available nutrients to support their rapid growth.
Now, the research team wanted to know the the role that calcium uptake by mitochondria plays in cancer cell metabolism and viability.
The team showed that interrupting the transfer of calcium from the endoplastic reticulum to the mitochondria in cancer cell lines of breast and prostate, as well as transformed human fibroblasts, resulted in impaired ATP production and activation of autophagy, in a similar fashion to healthy cells.
However, this counteraction, while sufficient for ensuring normal cell survival, yields different results in cancer cells due to their quick rate of growth. Cancer cells responded with massive death rates, while normal cells survived. Once cancer cells were provided with mitochondria metabolic substrates, researchers were able to rescue the lethal effect of inhibiting mitochondrial calcium uptake.
“This suggests that cell death was induced by compromised bioenergetics,” Foskett said.
Translating their findings in vivo, researchers showed that inhibiting the activity of IP3R channels led to a significant suppression of melanoma tumor growth in mice.
“Our findings reveal a fundamental and unexpected dependency by cancer cells on calcium transfer by IP3R channels into mitochondria for their viability,” Foskett said. “Mitochondria inside cancer cells are addicted to calcium. This addiction can now be considered as a target for new cancer therapies.
“Our studies suggest the existence of completely unexpected new targets for which drugs could be developed to kill cancer cells specifically by targeting calcium release from the ER and calcium uptake by mitochondria. A major challenge now is to discover drugs that can do this,” Foskett said.






