Genetic Mutations Affecting Protein Production Identified in Mitochondrial Disease
Mutations in an enzyme complex essential for mitochondrial protein production are a newly found cause of mitochondrial disease, researchers found.
The study, “Pathogenic variants in glutamyl-tRNAGln amidotransferase subunits cause a lethal mitochondrial cardiomyopathy disorder,” was published in the journal Nature Communications.
Mitochondria play an essential role in generating energy for all the functions of a cell and thus sustain organ function. They are present in almost every cell, and multiple genes within the mitochondria must function correctly for proper energy generation. Failure to do so causes mitochondrial disease characterized by energy depletion, organ failure, and accumulation of lactic acid (lactic acidosis).
Mitochondrial disease is inherited. Researchers from the University of Colorado analyzed mitochondrial genes in nine patients from five families that had infants with mitochondrial disease in an attempt to identify previously unknown mutations.
The infants had very high levels of lactic acidosis and severe cardiomyopathy, a condition in which the heart muscles are too weak to pump blood correctly. The symptoms appeared prenatally or within two to five months of birth and led the doctors to suspect mitochondrial disease. None of the infants survived longer than 6.5 months.
To identify the mutations, the team used whole-exome sequencing (WES), a technique that helps decipher the DNA sequence that carries the message for the final protein product.
They discovered mutations in genes that encode the glutamyl-tRNA amidotransferase protein complex (GatCAB), a key player in producing proteins that regulate energy production.
The GatCAB protein complex consists of three protein subunits — GatA, GatB, and GatC — encoded by genes QRSL1, GATB, and GATC respectively. Combining data from all five families, mutations were observed in all three genes.
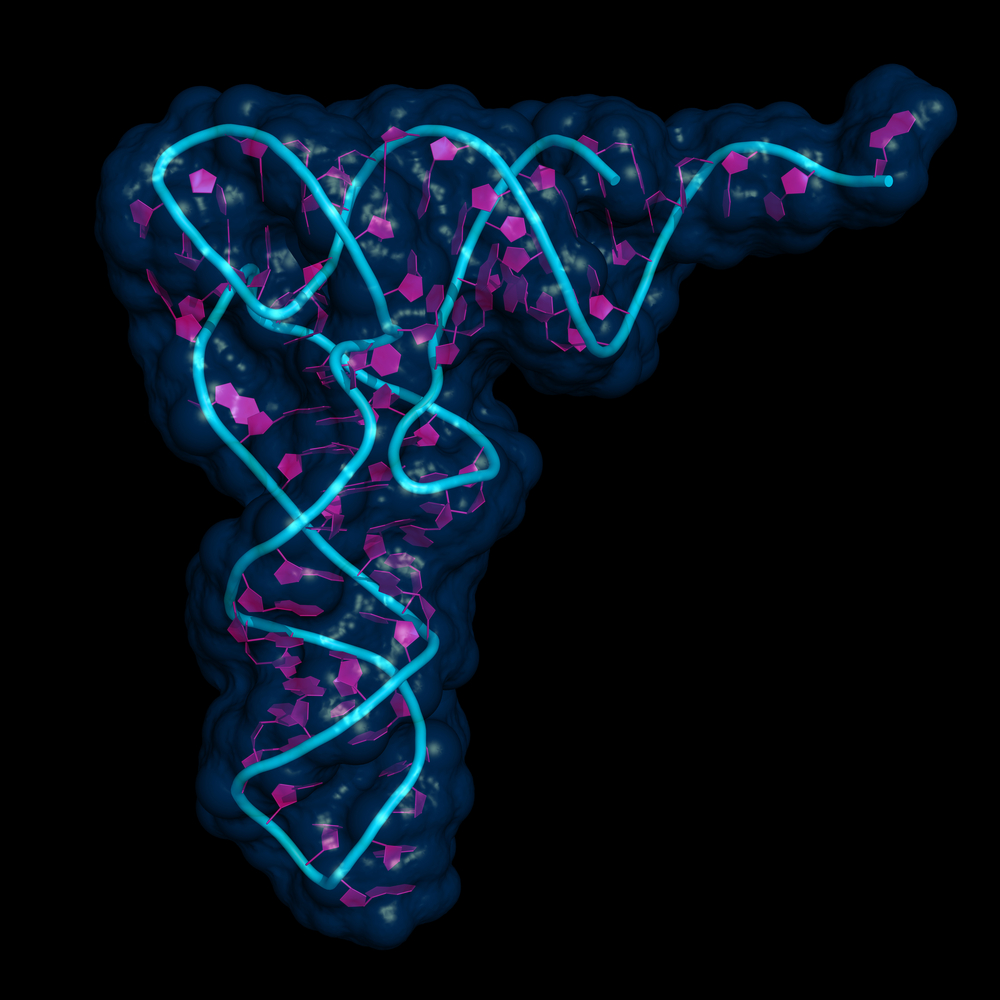
The message encoded by DNA is first converted to messenger RNA (mRNA). The mRNA is a string of nucleotides read by transfer RNA (tRNA) to generate the protein code called the amino acids. Each tRNA is specific to a particular amino acid and this process is mediated by different enzymes. The GatCAB is one such enzyme in mitochondrial protein synthesis required for correct processing of glutamyl tRNA.
The scientists used computer simulations to introduce the identified mutations in the GatCAB protein model and evaluated the impact of the mutations on the function of the protein. They observed that the mutations rendered GatCAB dysfunctional, thus establishing the disease-causing nature of these variations.
Researchers obtained fibroblasts (cells that support the structural framework of any organ) from the infants either during a biopsy or postmortem to evaluate mitochondrial function. They found that in the fibroblasts, the vital step for correct mitochondrial protein synthesis catalyzed by GatCAB — aminoacylation of glutamyl tRNA — was perturbed, thus affecting the levels of the amino acid glutamine (the amino acid specific to glutamyl tRNA). This, in turn, produced a defective protein.
The mitochondrial defect was more predominant in heart tissues compared with the fibroblasts, in line with the high energy demand of the tissue.
In the presence of glutamine, the defect was reversed. Thus, supplementing the lacking amino acid could “guide potential future therapeutic opportunities in disorders of translational [protein production] defects,” the authors wrote.
“Reduced mitochondrial translation and the ensuing effect on respiratory functions correspond to the clinical phenotype, consisting of cardiomyopathy and lactic acidosis with early lethality, regardless of the subunit involved,” the team concluded.






