Researchers Identify New Gene Variant Related to Childhood Mitochondrial Disease
Researchers used next-generation sequencing to identify NDUFB8 as a relevant gene in childhood-onset mitochondrial disease, a new study shows.
The study, “NDUFB8 Mutations Cause Mitochondrial Complex I Deficiency in Individuals with Leigh-like Encephalomyopathy,” was published in the American Journal of Human Genetics.
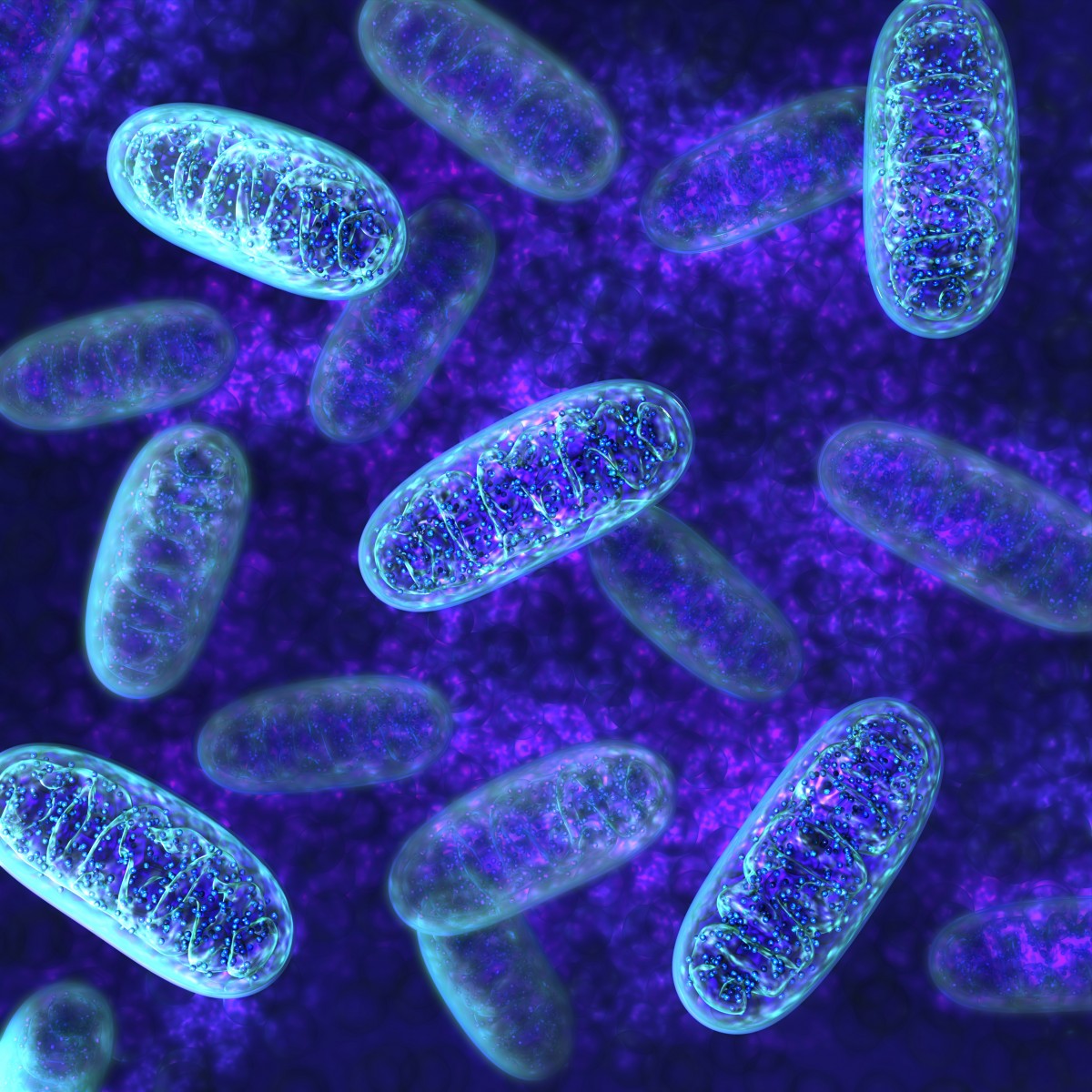
Respiratory chain complex I, one of the largest membrane-bound protein complexes in human cells, is essential for metabolism. Respiratory chain complex I deficiency is the most frequently identified biochemical defect in childhood mitochondrial diseases, accounting for 20% to 30% of all cases.
Clinical symptoms of these diseases include fatal infantile lactic acidosis, cardiomyopathy (heart disease), encephalopathy (brain disease), myopathy (muscle disease), and hepatopathy (liver disease). Leigh syndrome and Leber hereditary optic neuropathy are examples of diseases that are often associated with complex I deficiency.
Mammalian complex I is composed of 44 different subunits. To date, mutations have been reported in 27 complex I subunits. Whole-exome sequencing (WES) is a next-generation sequencing technique that has become an important tool in the identification of mutations that underlie complex I deficiency and the discovery of novel disease genes that cause this condition.
Gene mutations can lead to diseases because genes provide instructions to make a molecule called mRNA, which is then used to make protein. If the gene sequence is incorrect due to a mutation, then both the mRNA and the protein will be incorrect and unable to carry out their intended function. Therefore, determining which genes are mutated can help narrow down the cause of disease in individuals.
Researchers conducted WES on one mitochondial disease-affected person (P1) and targeted exome sequencing on a second affected individual (P2) from two unrelated families.
P1 was found to have isolated complex I deficiency, and P2 had reduced activity of complex I. Both patients had a progressive course of disease with encephalomyopathic features, including muscular hypotonia (low muscle tone), cardiac hypertrophy (enlarged heart), respiratory failure, failure to thrive, and developmental delays.
After WES was conducted, researchers looked for bi-allelic mutations in the genome, which refers to mutations that are present on both copies of a gene, the maternal and paternal copies.
In P1, researchers narrowed the search down to one gene that provides instructions to make a complex I accessory subunit, NDUFB8, which had two mutations. The first mutation was called “c.227C>A” and the second was “c.432C>G.” Both of these mutations lead to the production of an incorrect NDUFB8 protein, which was unable to carry out its function.
In P2, the genetic defect was identified by sequencing 215 specific genes that are known to have associations with mitochondrial disorders. Once again, a bi-allelic mutation search resulted in the identification of the gene NDUFB8. The two mutations in P2 were “c.184T>C” and “c.189delA,” which resulted in a nonfunctioning NDUFB8 protein.
Researchers then further investigated the importance of this gene by adding the correct version of the NDUFB8 gene into cells that were obtained from affected individuals. This experiment restored mitochondrial function, which confirmed that NDUFB8 mutations are the cause of complex I deficiency in these individuals.
“Using next generation sequencing, we identified deleterious NDUFB8 mutations in two complex I-deficient individuals,” the authors concluded. “Our findings broaden the etiology of complex I deficiency and reveal NDUFB8 as an essential component for the stability and activity of complex I.”






