Scientists Seek Better Understanding of Neurodegeneration by Looking at Mitochondrial Interaction
Researchers have discovered a key piece of information that may advance knowledge of how interactions between mitochondria and other structures contribute to neurodegeneration.
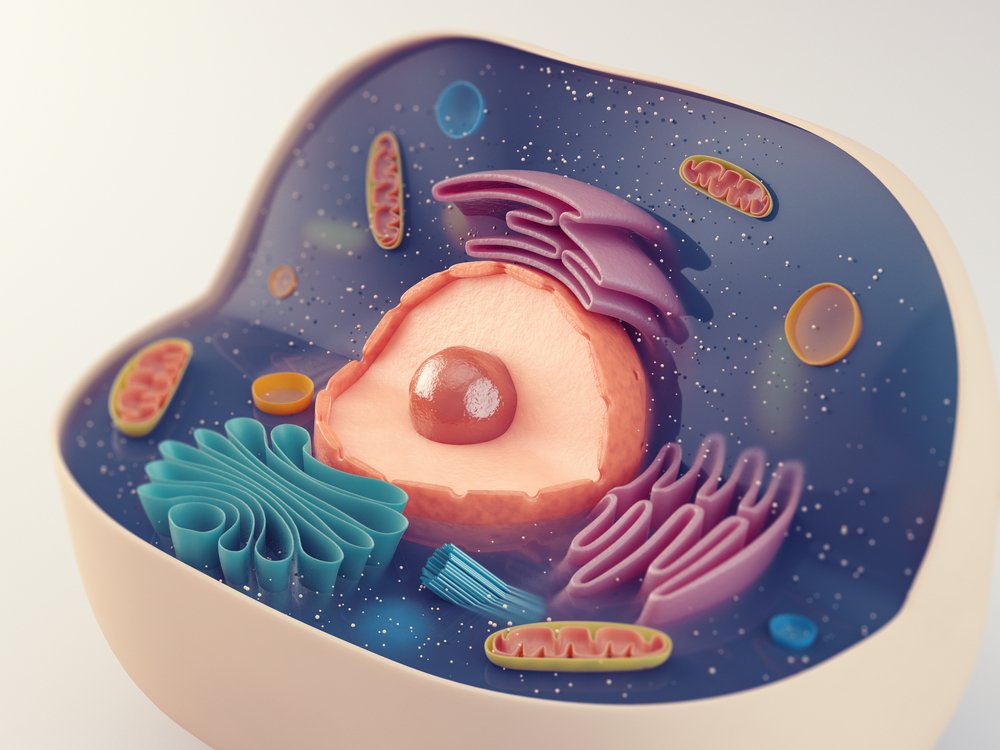
A study published in the Journal of Biological Chemistry identified specific proteins that are required for interactions between mitochondria and the endoplasmic reticulum (ER), which is responsible for making proteins, among other tasks.
With these insights, researchers are now preparing to study if these interactions are abnormal in people with neurodegeneration by comparing nerve cells from patients and healthy people.
To gain this initial knowledge, researchers behind the study, “Ascorbate peroxidase proximity labeling coupled with biochemical fractionation identifies promoters of endoplasmic reticulum mitochondrial contacts,” developed a new method that allowed them to examine interactions between cell components, or organelles.
“Think of [an organelle] like a ferry docking at one site, unloading and loading passengers and cars, and then going to another site and doing the same thing,” Jeffrey Golden, a professor at Brigham and Women’s Hospital and Harvard Medical School and senior study author, said in a press release.
“Their ability to dock, load, and unload cargo requires guides or ramps of specific width and heights that connect the boat and land or they cannot freely load and unload.”
These docking sites — enabling the exchange of molecules and communication — are crucial for mitochondria and other cell components to function normally.
While researchers have looked at how these interactions work in simple organisms, such as yeast, they realize that these processes are far more complex in mammals.
To allow for studies of how mitochondria and ER exchange information and matter, researchers adapted a newly developed method for studies of protein interactions. The method makes use of an enzyme called APEX, or ascorbate peroxidase.
APEX works by attaching biotin to nearby proteins. By genetically engineering mitochondria that had APEX on their surface, they designed a system that would enable mitochondria to label proteins they came very close to, with added biotin.
Using lab-grown cells, they allowed mitochondria to interact as usual with the ER. Researchers could then identify the specific ER proteins that had taken part in this interaction, as they had biotin attached.
“It was previously feasible to only look at one molecule at a time to assess what it interacted with,” Golden said. “The method we have used is more rapid and allows an unbiased look at a whole system and what’s happening at that organelle’s interface.”
One of the proteins that turned up in the screen was RTN1a. Researchers said it is possible that this protein could be involved in neurodegenerative disease processes. But so far, the findings only allow for speculation. Particularly since the experiments were performed in kidney cells.
To find out, researchers need to study neurons from patients and healthy people to identify potential flaws in how the protein function — a project they will now pursue.
“Does the liver use the same proteins to control these kinds of interactions that neural cells do? Is one [protein] more important for calcium exchange and another set of proteins more important for lipid exchange? I think there’s a lot of cell biology that we just don’t know and could be answered” using this method, Golden said.






