Increased Urea Levels Trigger Inflammation and Mitochondrial Dysfunction, Study Finds
Uremia (increased blood urea levels) may promote inflammation in the adipose tissue (fat) and faulty mitochondrial activity in the muscle, which can contribute to the development of end-stage renal disease, new research indicates.
The study, titled “Uremia induces adipose tissue inflammation and muscle mitochondrial dysfunction,” was published in the journal Nephrology Dialysis Transplantation.
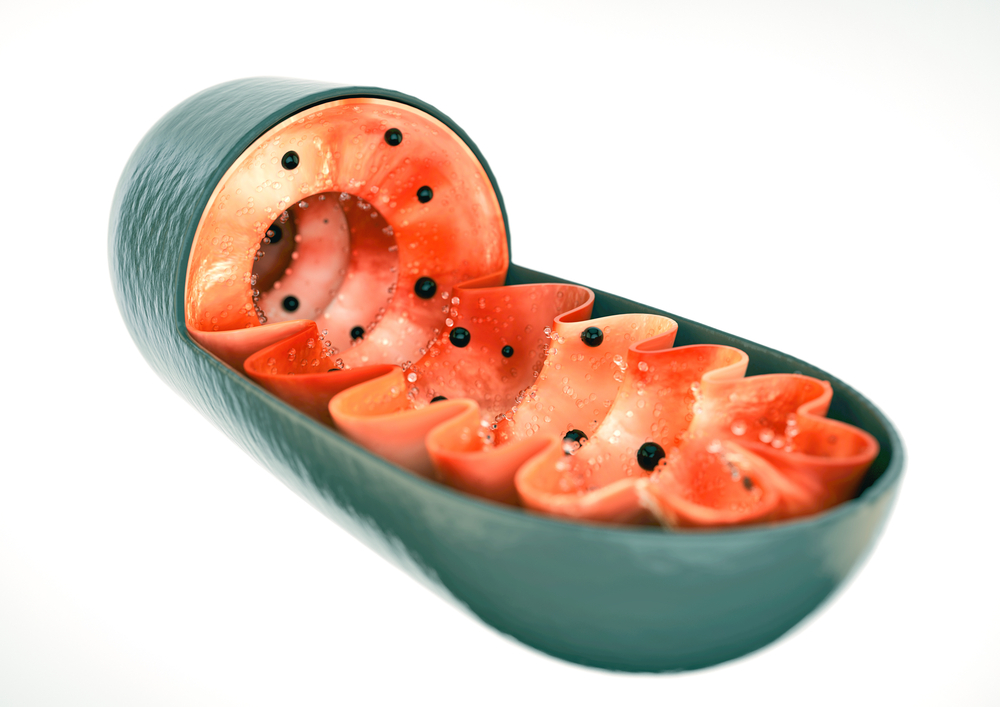
Previous studies have shown that end-stage renal disease (ESRD) is associated with inflammation and increased levels of reactive oxygen species (ROS), a group of molecules produced during mitochondrial activity that cause damage to cell components. Uremia is considered the terminal clinical manifestation of ESRD and is associated with several complications that result in patient morbidity and even mortality.
“Uremia and inflammation affect muscle function as well as adipose tissue metabolism,” researchers wrote. “Muscle wasting is common in ESRD patients and is associated with significant morbidity.”
The objective of the study was to assess whether there are any tissue markers of inflammation and abnormal mitochondrial activity associated with uremia and leading to ESRD.
Researchers used samples of adipose and muscle tissue from 18 ESRD patients and six healthy individuals. They found that inflammation markers, such as the higher presence of immune system’s cells, were higher in samples of adipose tissue from ESRD patients than they were in control individuals. Mitochondrial activity (low presence of mitochondrial proteins) also was lower in these patients.
In cultured muscle cells exposed to high levels of urea, mitochondrial activity also was reduced. However, researchers were able to rescue it by stimulating cells with a compound called N-acetyl cysteine.
They observed that inflammatory molecules such as TNF-alpha and interleukin-6 also promoted low mitochondrial function, but this was reversed with adiponectin, a protein naturally produced by fat cells.
Together, these results suggest that inflammation and oxidative stress/faulty mitochondrial activity are implicated in ESRD, and that adipose tissue may play an important role in mediating uremic inflammation.
“In sum, our study suggests that the adipose tissue of … ESRD patients contributes to uremic chronic inflammation and that inflammation and ROS play a role in mitochondrial dysfunction seen in uremia,” researchers wrote. “Further studies are needed to delineate the mechanism of adipose tissue inflammation and mitochondrial dysfunction in uremia.”






