Cell-reprogramming Method Developed to Test Approved Therapies on Mitochondrial Disease
Scientists have developed a way to potentially treat mitochondrial disease — and it involves reprogramming patients’ cells.
In “Human iPSC-Derived Neural Progenitors Are an Effective Drug Discovery Model for Neurological mtDNA Disorders,” researchers explained that they reprogrammed patients’ cells, then used them to test U.S. Food and Drug Administration (FDA)-approved medications to determine whether any could apply to mitochondrial disease. The results were published in the journal Cell Stem Cell.
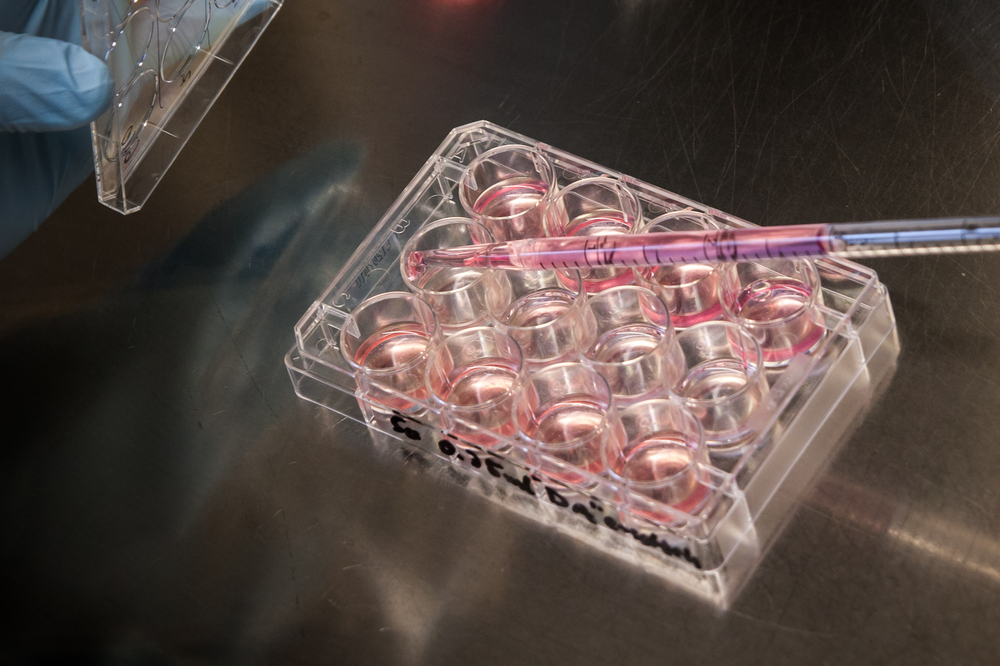
Researchers extracted skin cells from patients with faulty mitochondria and reverted them to a more basic type of cell, called induced pluripotent stem (IPS) cells. They can then be “reprogrammed” into neural progenitor cells.
“It was crucial to establish a cellular system with similar characteristics of the affected nerve cells in the patients,” said Alessandro Prigione, MD, PhD, who led the team of researchers at Max Delbrueck Center for Molecular Medicine in Berlin. “We discovered that neural progenitor cells show properties that can be associated with the disease and were perfectly suitable for use in large-scale drug screens.”
Tests showed the neural progenitor cells had all of the properties associated with mitochondrial disease, including the calcium imbalance and reduced energy production observed in patients.
“Once you have a good model system, you can screen the several thousand drugs already approved by the FDA,” Prigione said in a press release. “This creates the potential of developing truly personalized treatments — even for very rare diseases.”
The researchers have tested 130 FDA-approved substances. One medication, Stendra (avanafil), which is used to treat erectile dysfunction, reversed some of the cellular imbalances mitochondrial defects caused.
Prigione said the team is preparing a clinical trial to test the medication in mitochondrial disease.






