Mitochondria Control Renewal of the Intestinal Wall, Development of Gut Diseases, Study Finds
Mitochondria present in cells of the inner intestinal wall control the renewal of this organ’s surface and may contribute to the development of gut diseases, according to a new study published in the journal Nature Communications.
The study, “Mitochondrial Function Controls Intestinal Epithelial Stemness And Proliferation,” was conducted by a research team from the Technical University of Munich.
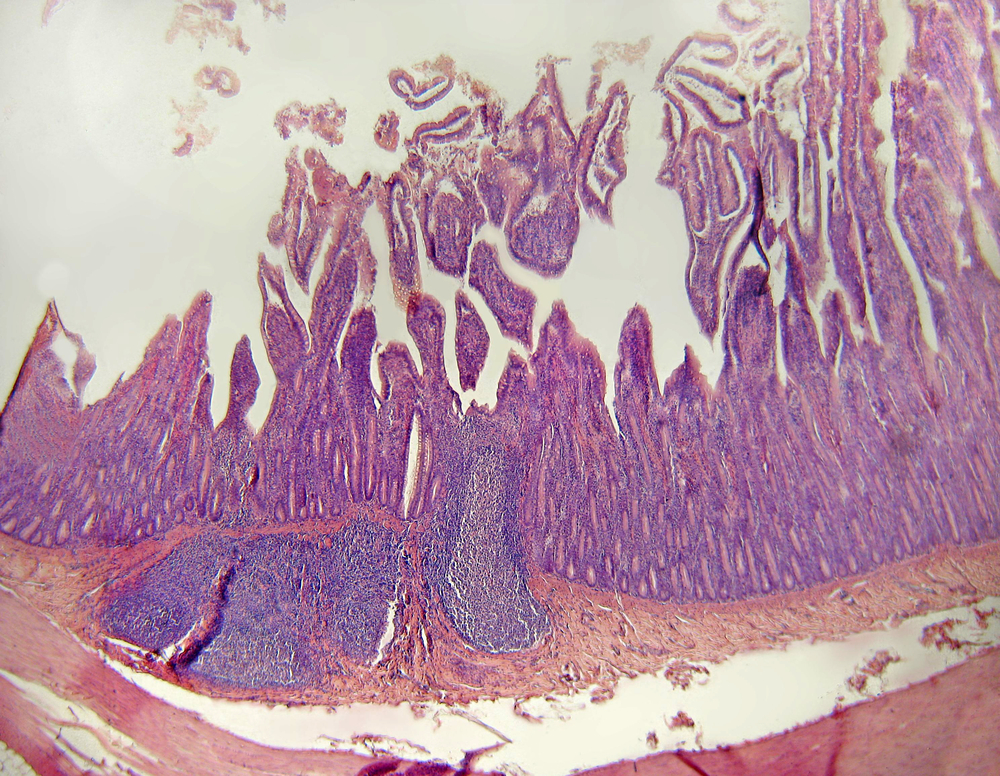
Mitochondria are the cell’s compartments where energy is produced to supply all necessary functions of the body. One such function is the complete renewal of the inner intestinal wall, a surface full of tiny bumps, that occurs every four to five days. This process is guided by stem cells, a group of immature cells that can become other cell types in the body – in this case, cells of the intestine’s wall.
Given the crucial role of the mitochondria as energy suppliers, when these organelles are defective within the intestinal surface cells, the self-renewal of the intestinal wall is interrupted, which, under extreme conditions, may result in chronic inflammation.
In conditions of cellular stress, cells activate a group of proteins, called chaperones, to ensure the proteins involved in the renewal process are properly produced within the cells to maintain the equilibrium of the intestinal mucosa. Among chaperones, the HSP60 protein is one essential regulator of mitochondrial activity in cells of the intestinal surface.
Researchers used mice depleted of HSP60 to investigate in detail exactly how important is the function of this protein to the renewal of the intestine’s wall and how mitochondria react in cells that do not have the protein. They observed that cells depleted of HSP60 activate a stress response in the mitochondria, called the mitochondrial unfolded protein response (MT-UPR), leading to mitochondrial dysfunction. This caused a reduction in energy production in these cells, which lost their ability to multiply and complete the regeneration process. However, this cellular stress signaled surrounding cells with working mitochondria to start growing.
“The reaction to the lack of HSP60 was startling because although stem cells lost their characteristic properties, the stressed cells in the surrounding intestinal mucus wall activated a growth program leading first to hyperproliferation that finally ended in tissue regeneration,” Dirk Haller, PhD, senior investigator of the study, said in a press release.
This happened because cells with no HSP60 and with dysfunctional mitochondria send out growth factors to the surrounding cells “calling for help,” and ensuring that cells that still have intact mitochondria multiply and replace the affected ones.
The results obtained in this study showed that lack of HSP60 induced a communication process among stem cells in the intestine that allowed the activation of a previously unknown healing mechanism. This information can be of great relevance for the development of treatments for intestine injury or inflammation. Importantly, it also uncovered a mechanism through which cells that are under permanent stress or inflammation can trigger the development of cancer by inducing the growth of other cells.
“This shows what a fundamental role functioning mitochondria have in regulating intestinal tissue renewal and how they might contribute to chronic intestinal diseases,” said Haller.






