Modified Atkins Diet Can Cause Muscle Damage in People with Mitochondrial Myopathy, Study Finds
A Finnish study of a modified Atkins diet, a popular high‐fat/low‐carbohydrate diet, in a small group of people with mitochondrial myopathy (MM) and progressive external ophthalmoplegia (PEO) found the diet induced progressive muscle pain and damage within two weeks, and the researchers suggest that patients using such diets to control disease symptoms be closely monitored.
The study, “Modified Atkins diet induces subacute selective ragged‐red‐fiber lysis in mitochondrial myopathy patients,” was the result of collaborative research effort involving several institutions, and published in EMBO Molecular Medicine.
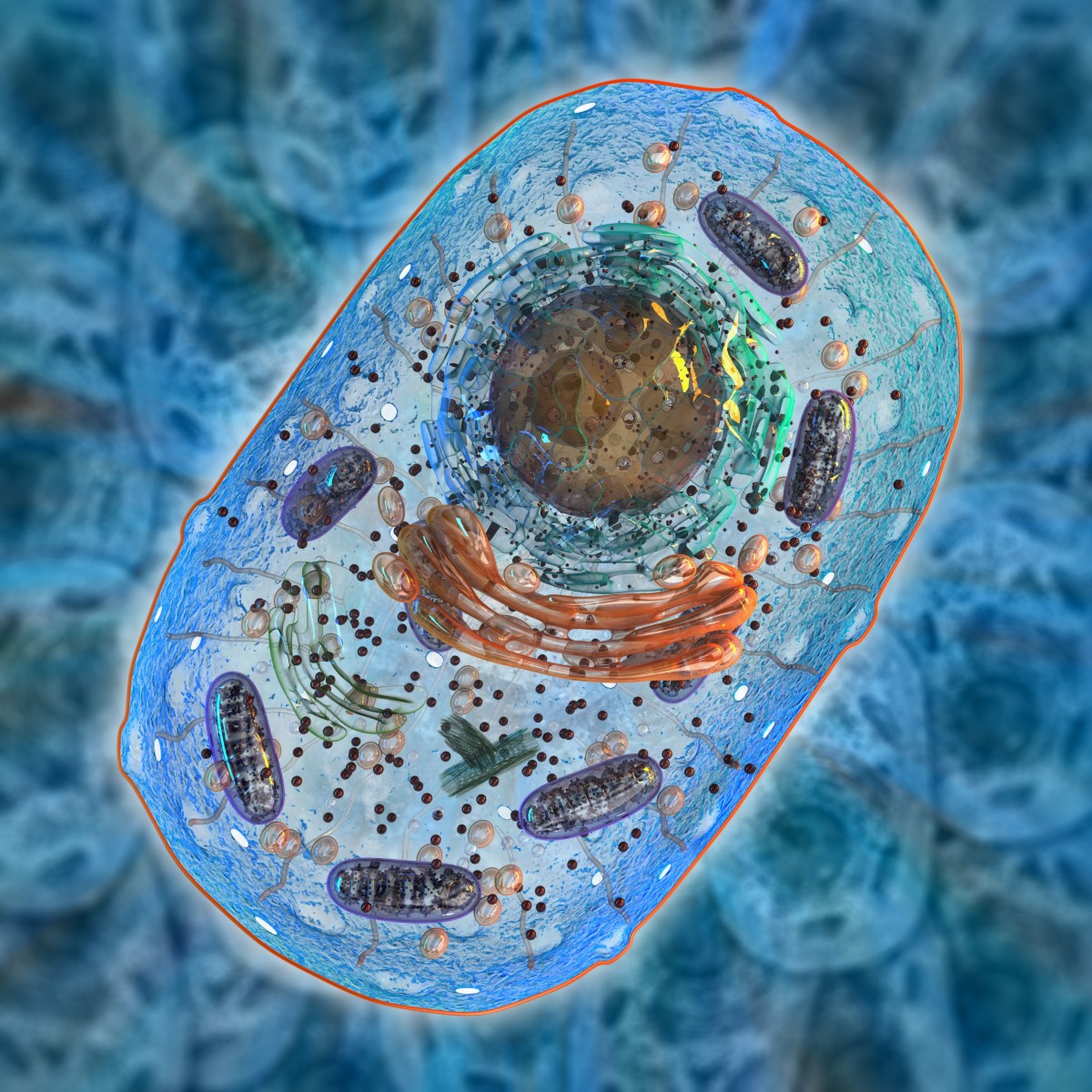
Mitochondrial myopathy with progressive external ophthalmoplegia (PEO/MM) is a common feature of dysfunctional mitochondria, the cell part responsible for converting the energy of food to power most cell functions. The disease is characterized by mild visual impairment and muscle weakness, which usually manifests in the early adulthood.
There is no cure for PEO/MM but several routes have been suggested to ameliorate the symptoms. This includes diet, and some animal studies have proposed that a high‐fat/low‐carbohydrate diet can ease disease symptoms. Such findings have previously not been verified in patients.
Researchers assessed the effects of a high‐fat/low‐carbohydrate modified Atkins diet, or mAD, in a total of five people with mild proximal muscle weakness and exercise intolerance, and in 10 gender- and age-matched healthy controls, two for each patient. Participants were given a normal, standard diet for two weeks, then gradually switched to mAD for four weeks, and clinical manifestations were accordingly assessed.
Results found that all five patients experienced progressive muscle pain and deterioration after 1.5 and 2 weeks of starting the diet, leading to its early discontinuation. Analysis of muscle structure showed fiber damage noticeable through the rough and irregular recorded morphology of the fiber, called ragged‐red‐fibers (RRFs). These irregularities seemed to be partially regenerated and restored, according to the follow-up made at 2.5 years later.
“Our results indicate that nutrition can drastically modify progression of MM and that RRFs are dependent on carbohydrate supply. Furthermore, our results show that mAD may induce muscle cell damage in a small population group with subclinical mitochondrial disease,” the researchers concluded.
“Based on our results, muscle symptoms and creatine kinase values should be closely monitored if low‐carbohydrate diet is used as treatment for mitochondrial disease patient. The uniform response of our PEO patients to mAD indicates existence of a yet‐unknown metabolic block in adult‐onset MM. The exciting potential of dietary intervention as a treatment of MM/PEO, aiming to target and reduce the number of RRFs, requires further investigation,” they added.






