Distinguishing Between Primary and Secondary Mitochondrial Disease Important for Diagnosis, Treatment
A recent review highlights the latest findings in mitochondrial disease and the importance of distinguishing between primary mitochondrial disease (PMD) and secondary mitochondrial disease (SMD) in the diagnosis of patients, as treatments and outcome may be very different for these two cases.
The study, “Primary Mitochondrial Disease and Secondary Mitochondrial Dysfunction: Importance of Distinction for Diagnosis and Treatment,” conducted by Dr. Dmitriy Niyazov, MD, and colleagues from different research institutions in New Orleans and Arkansas, was published in the journal Molecular Syndromology.
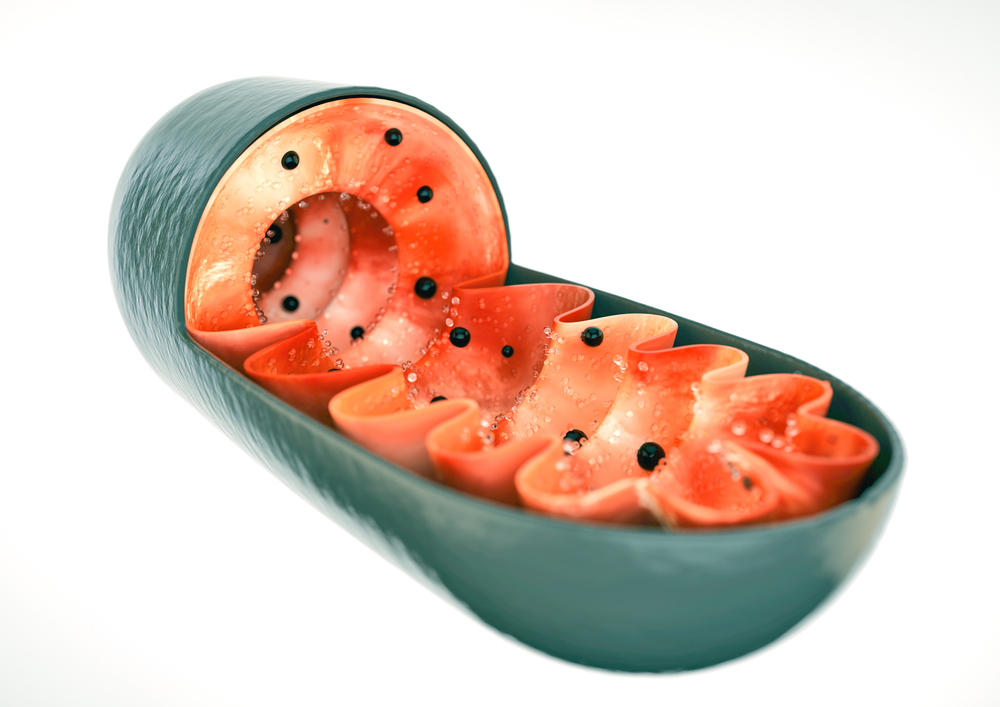
In general, mitochondrial disease refers to a group of disorders that result from abnormal energy production by mitochondria, the cell’s powerhouse. Recent advances in genetic testing have shown that mitochondrial dysfunction can be even more complex than has previously been assumed.
Primary mitochondrial disease (PMD) is clinically diagnosed and, when possible, confirmed by the identification of pathogenic mutations in mitochondrial DNA (mtDNA) or nuclear DNA (nDNA). These mutations usually affect proteins involved in reactions of oxidative phosphorylation; that is, the reactions necessary for energy production in the mitochondria.
However, many disorders show similar effects in terms of abnormal mitochondrial function, but are elicited by mutations in other genes not related to oxidative phosphorylation reactions. These cases are referred to as secondary mitochondrial disease (SMD) and can be either inherited or acquired due to adverse environmental conditions.
“SMD can be inherited or acquired, which is an important distinction from PMD, which can only be inherited,” the authors wrote in their report. “Distinguishing whether mitochondrial dysfunction is inherited or acquired is extremely challenging, and at present, the best method for making this distinction is still poorly understood.
“One of the most reliable (but not all-encompassing) tools in this daunting task is comprehensive molecular testing of both mtDNA and nDNA which, at least in some cases, can ultimately distinguish between PMD and SMD,” they wrote.
According to the authors, the diagnosis of PMD and SMD is based on one or several mitochondrial disease criteria (MDC) scoring systems designed to diagnose the energy-producing mitochondrial function. These include Nijmegen, modified Walker, Morava criteria and others that assess biochemical, clinical, tissue, and molecular characteristics, rating certain clinical or laboratory findings into definite, probable, possible, or unlikely diagnosis of mitochondrial disease.
Unfortunately, PMD and SMD can have overlapping symptoms and signs, which makes a clear diagnosis hard to obtain.
“(…) in our opinion (in absence of consensus guidelines), the MDC scoring systems, while imperfect, currently represent the best guidance on the minimal diagnostic criteria sufficient to diagnose PMD or SMD,” the authors wrote. “In other words, certain minimal clinical phenotype and/or genotype (combination of symptoms, signs, and tests) should be considered to diagnose a patient with PMD or SMD for clinical purposes, given that a vast majority of patients do not perfectly fit all the MDC components.”
In their study, the authors also review several disorders associated with SMD, such as neuromuscular disorders, autism, neurodegenerative disorders, and cancer, which support the theory that SMD is likely much more common than PMD. Such findings have to be considered when designing therapies for these disorders.
The authors also report the case of a female child with SMD caused by a genetic mutation whose condition improved after a treatment that included changes in nutrition and a regular exercise program.
“While we advocate treating both PMD and SMD using diet, exercise, and specific vitamin supplements, it is crucial to identify a possible non-mitochondrial etiology, since it may require separate treatment to decrease morbidity and mortality,” the authors wrote. “The standard interventions for PMD should be strongly considered, while new, more effective treatments such as gene therapy are being investigated.”
“In our opinion, standard treatment used in PMD can be effective for some individuals with non-PMD disorder and SMD, and given their safety and availability, systematically starting such treatments, even without a firm diagnosis, is reasonable,” they wrote.






