Study Shows Mitochondrial DNA, Nuclear Gene Interaction May Provide Clues to Mitochondrial Diseases
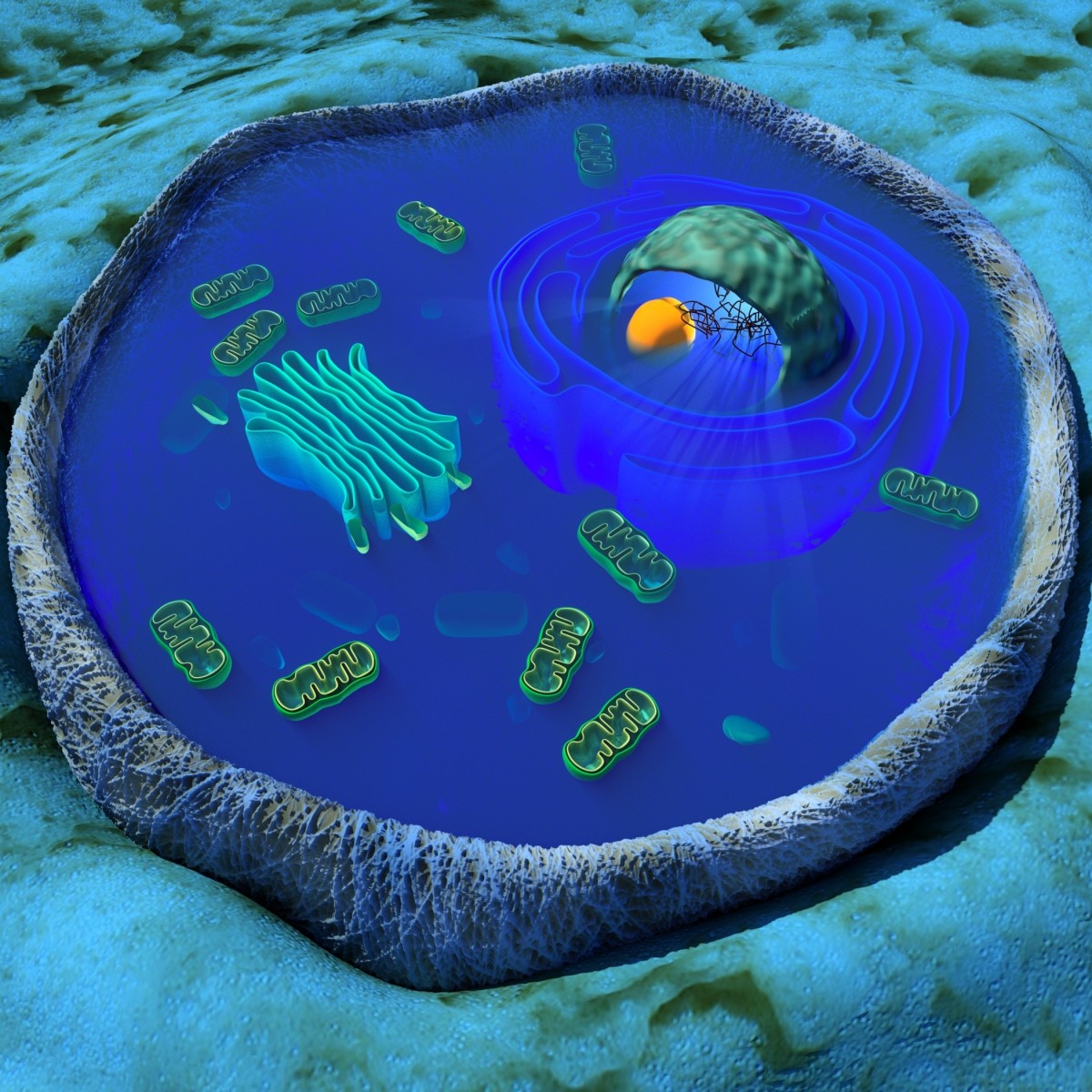
Researchers from New Zealand have shown for the first time that mitochondrial DNA (mtDNA) can leave the mitochondria, travel to the nucleus, and establish interactions with specific genes.
Findings from the study “Interactions between mitochondrial and nuclear DNA in mammalian cells are non-random,” published in the journal Mitchondrion, may provide novel insights on how mitochondria dysfunction affects cellular processes that are not directly related to energy production. The findings could lead to discoveries in many mitochondria-related diseases.
“We found evidence that mitochondria DNA and nuclear DNA ‘talk to each other’, and these interactions aren’t random,” Justin O’Sullivan, a molecular geneticist at the University of Auckland Research Institute and study’s lead author said in a press release.
Mutations in mtDNA are commonly linked to a variety of debilitating diseases including heart disease, neurodegenerative diseases, diabetes, deafness, and eye disorders. Because mitochondria are the cell’s powerhouse, researchers often hypothesize that mitochondrial diseases are caused by an insufficient energy production that impairs the cells from working properly.
The recent findings suggest that there may be another possible explanation: mutations in mtDNA affect the way mtDNA and nuclear DNA “talk” to each other.
Although it is not fully clear how the two sets of DNA communicate with each other, or the effects of that communication, the researchers believe that such interactions may regulate the expression of particular sets of genes in the nucleus as was previously shown in yeast. This may explain how mitochondria are involved in cellular processes that are not directly related to energy generation such as cellular differentiation, cell growth, and cell death.
“We think the connections we detected are part of a feedback system between mitochondria and the cell nucleus that may influence how humans grow and develop throughout life,” O’Sullivan said. “We know that these connections between mitochondrial and nuclear DNA can influence how the nuclear genes work in yeast, and we speculate that the same occurs in humans.”
The most accepted theory regarding the origin of the mitochondria is that a bacteria that could use oxygen to survive, the mitochondria precursor, was engulfed by a host cell that could not function in the presence of oxygen and that a symbiotic relationship was established between the two. That is why mitochondria have their own DNA.
But over the course of evolution the mitochondrial genome has dramatically reduced and presently more than 1,000 proteins required for mitochondrial function are encoded by the nuclear DNA. The researchers believe that these interactions may also be occurring between nuclear DNA and DNA that was historically derived from the mitochondria so that there is a coordinated expression of the genes to allow functional mitochondria to assemble.
“This study adds to our understanding of the way in which changes to mitochondria manifest as disease. Further research could yield new treatment avenues,” study co-author and associate professor, Mark Vickers, from the Liggins Institute, University of Auckland, concluded.






