In Vitro Study Shows Positive Effects of Ketogenic Diet on Mitochondrial Function in Leigh Syndrome
Researchers recently tested the effects of the high-fat, low carbohydrate ketogenic diet on fibroblasts from patients with Leigh syndrome (LS), focusing on decanoic acid. The results suggest that this component had beneficial effects on mitochondrial function, decreasing reactive oxygen species (ROS) and improving mitochondrial respiration. Therefore, the effects of this diet should be investigated in animal models of mitochondrial disease.
The research paper, “The pleiotropic effects of decanoic acid treatment on mitochondrial function in fibroblasts from patients with complex I deficient Leigh syndrome,” was published in the Journal of Inherited Metabolic Disease.
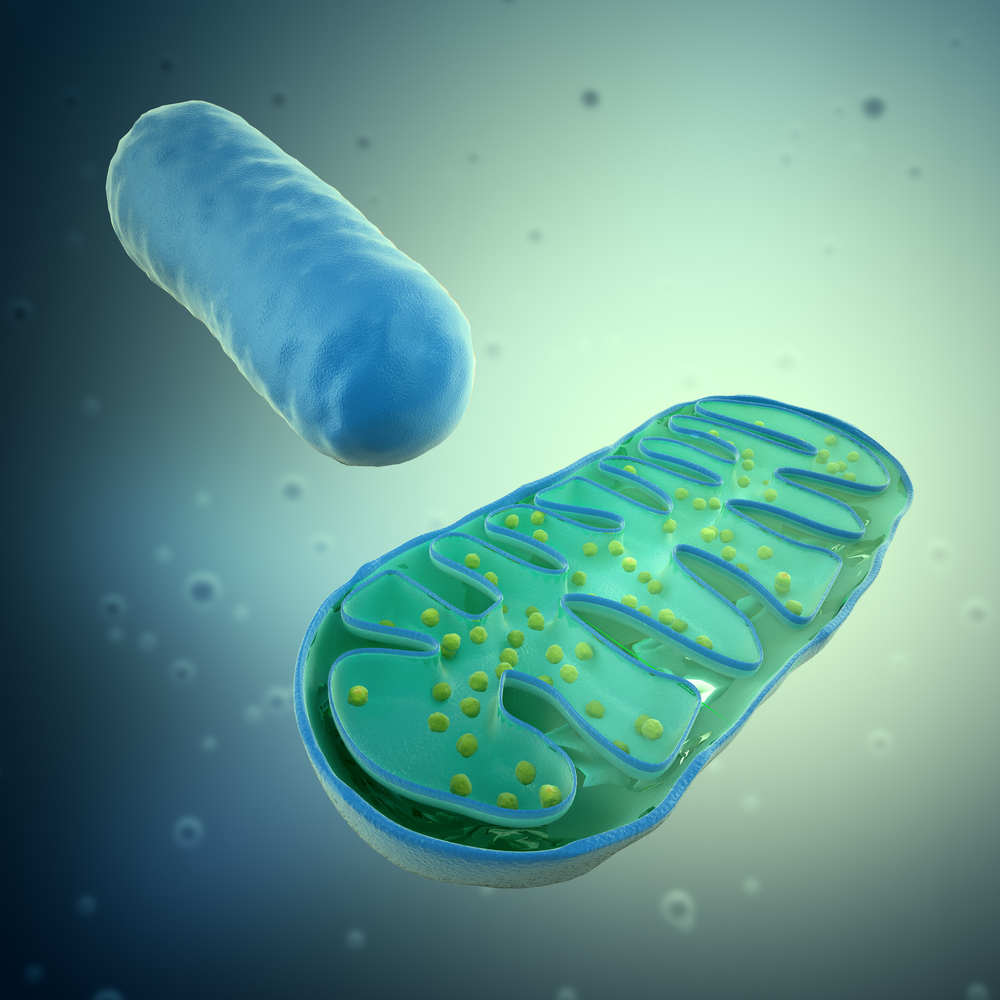
Mitochondrial diseases are the most common group of inherited metabolic disorders, consisting of a group of very diversified diseases, with varied degrees of severity and different genetic and phenotipic characteristic. Among these, Leigh syndrome (LS) is the most severe form of mitochondrial dysfunction, characterized by progressive neurological abnormalities starting in late infancy or early childhood. Despite the advancement of research in this area, treatment options for mitochondrial disease remain very limited and usually rely on the alleviation of symptoms.
The ketogenic diet (KD), a high fat and low carbohydrate diet, has been investigated as a potential treatment for patients with mitochondrial diseases, as research in animal models has shown that the diet increased mitochondrial respiration and decreased of reactive oxygen species (ROS). The medium-chain triglyceride (MCT) diet is a variation of the classic KD, where 60 percent of total caloric intake is fat instead of the 80 percent established for KD.
The effects of these diets are still not fully understood for patients, so in this study, the researchers focused on a promising component, decanoic acid (C10) — a component of the medium chain triglyceride KD — which has been shown to participate in mitochondrial biogenesis. The effects of C10 were investigated in fibroblasts recovered from LS patients and a series of assays helped the scientists determine the beneficial effects of this component. Results indicate that in 50 percent of the tested fibroblasts C10 increased markers for cellular mitochondrial content, while also increasing fatty acid metabolism and decreasing glucose metabolism. Importantly, oxidative stress was also decreased and cellular resistance to this harmful event also increased.
The researchers believe that this therapy should be further explored in mouse models of mitochondrial disease. “Our results also highlight the importance of genetically and phenotypically matched cohorts when studying treatments for mitochondrial diseases, and suggest that not every mitochondrial patient will benefit from the same type of treatment.
“Furthermore, the assay methods described here could be utilized to identify suitable patients for further investigation of the efficacy of C10 therapy in a clinical trial, in a ‘personalised medicine’ approach,” the authors conclude.






