New Nanoblade More Effectively Allows Engineered Mitochondria to Be Returned to Cells
A new nanoblade can open a cell’s membrane to insert mitochondria directly into the cytoplasm, allowing for scientists to manipulate mitochondria outside the cell before returning them. The technique, described in the study “Mitochondrial Transfer by Photothermal Nanoblade Restores Metabolite Profile in Mammalian Cells,” may have implications for therapeutic approaches against mitochondrial diseases.
The photodermal nanoblade is composed of a microscope, a laser, and a titanium-coated micropipette — the ‘blade’ — operated with a joystick controller. When a laser pulse is delivered to the micropipette, the titanium heats up and vaporizes the surrounding water layers, forming a bubble close to a cell. Bubble expansion and collapse generates a local force that punctures the cell membrane, creating a passageway for large cargo delivery that is rapidly repaired by the cell.
Researchers had previously used the nanoblade to transfer other components between cells.
“As a new tool for cell engineering, to truly engineer cells for health purposes and research, I think this is very unique,” said Mike Teitell, the study’s senior author and a pathologist and bioengineer at the University of California, Los Angeles (UCLA), in a press release. “We haven’t run into anything so far, up to a few microns in size, that we can’t deliver.”
Mutations in the mitochondrial DNA (mtDNA) are known to be involved in a number of familial diseases that affect tissues requiring high amounts of energy, such as the brain, heart, and muscle. However, unlike the nuclear genome, strategies for altering mtDNA are limited.
“There’s a bottleneck in the field for modifying a cell’s mitochondrial DNA,” Dr. Teitell said. “So we are working on a two-step process: edit the mitochondrial genome outside of a cell, and then take those manipulated mitochondria and put them back into the cell. We’re still working on the first step, but we’ve solved that second one quite well.”
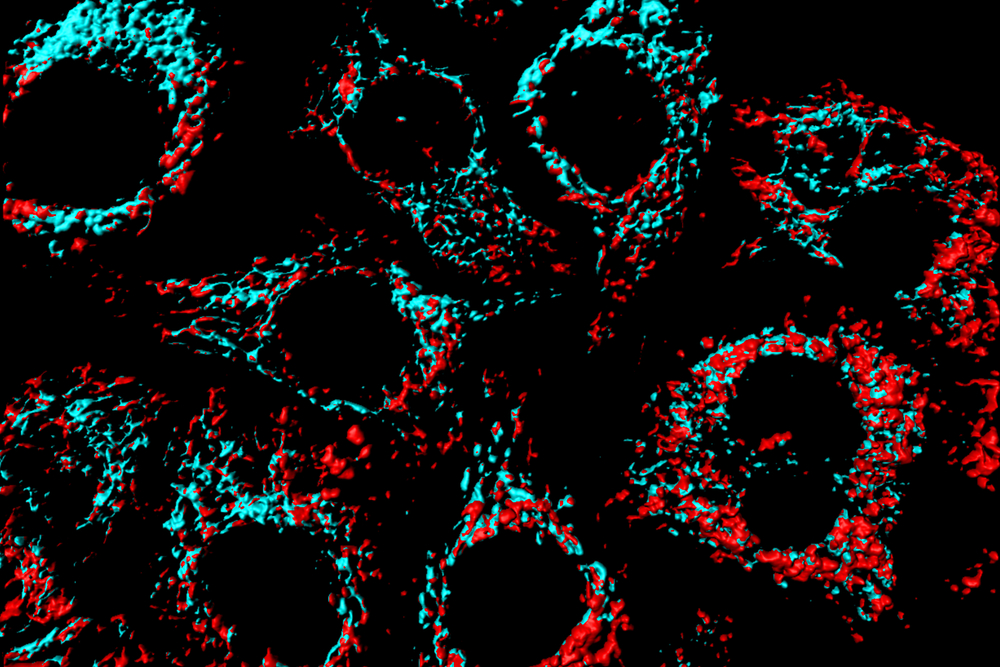
In the study, published in the journal Cell Metabolism, researchers used the nanoblade to insert tagged mitochondria from embryonic kidney cells or human breast cancer cells into cells that lacked mtDNA, and found that the mitochondria had been successfully transferred and replicated by 2 percent of the cells, a success rate that markedly exceeded the 0.001-0.5 percent obtained with other techniques that had been reported to work.
“The success of the mitochondrial transfer was very encouraging,” said Pei-Yu “Eric” Chiou, a bioengineer who together with Dr. Teitell came up with the nanoblade idea to transfer cell nucleus. “The most exciting application for the nanoblade, to me, is in the study of mitochondria and infectious diseases. This technology brings new capabilities to help advance these fields.”
The research team has already scaled up the nanoblade and made an automated high-throughput version; they hope to commercialize it and allow other scientists to use the technique.
“We want to make a platform that’s easy to use for everyone and allow researchers to devise anything they can think of a few microns or smaller that would be helpful for their research — whether that’s inserting antibodies, pathogens, synthetic materials, or something else that we haven’t imagined,” Dr. Teitell concluded. “It would be very cool to allow people to do something that they can’t do right now.”






