Parkinson’s Disease Shows Signs of Mitochondrial Dysfunction
A recent literature review revealed that mitochondria may play a role in the second most common neurodegenerative disorder: Parkinson’s disease (PD). The review was published in the International Journal of Molecular Sciences and is entitled “Mitochondria: A Therapeutic Target for Parkinson’s Disease?“.
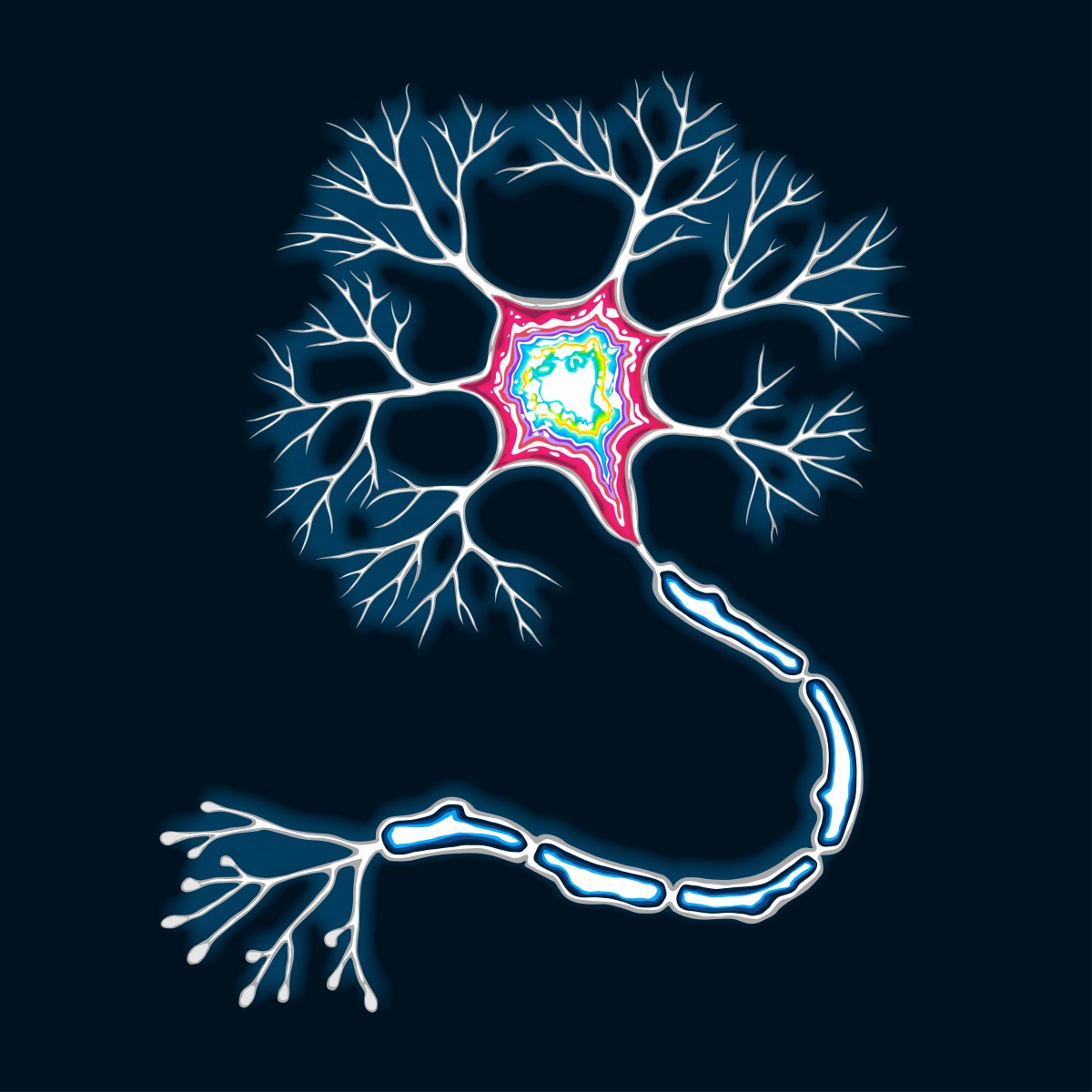
In PD, neurons that produce the neurotransmitter dopamine (dopaminergic neurons) are selectively degenerated. Multiple studies have found that mitochondrial dysfunction may be one reason why dopaminergic neurons die.
“The exact causes of neuronal damage are unknown, but mounting evidence indicates that mitochondrial-mediated pathways contribute to the underlying mechanisms of dopaminergic neuronal cell death both in PD patients and in PD animal models,” wrote the study’s lead author Dr. Yu Luo from Case Western Reserve University.
Interestingly, some of the basis of the association between mitochondria and PD lies in how animal models of PD are generated. It is common practice to use chronic systemic administration of rotenone to rats to induce a human-like PD state. Rotenone inhibits one of the mitochondrial proteins involved in the respiratory chain. Similarly, meperidine has been used in animal models of PD, and it is known to cause PD in humans.
Other reasons for mitochondrial dysfunction are based in the shape of mitochondria. These organelles are highly organized in a tubular network that is constantly changing its shape by undergoing fusion and fission. If either fusion or fission are not working correctly, the mitochondria can fragment, falter in energy production, and be more liable to oxidative stress. These effects can lead to dopaminergic neuronal cell death.
Additionally, within mitochondria, there is mitochondrial DNA (mtDNA) that encodes proteins involved in the respiratory chain. Any alteration in mtDNA is likely to cause mitochondrial dysfunction. Scientists have discovered mtDNA deletions in dopaminergic neurons isolated from deceased PD patients’ brains, and altering mtDNA in live animals leads to PD-like symptoms.
According to Dr. Luo, “targeting mitochondria may offer the opportunities for drug development to treat neurodegenerative diseases such as [PD].” With the knowledge that mitochondria may play a role in PD progression, a handful of therapeutics are potential candidates for PD treatment. These include small-molecule inhibitors of defective proteins in PD, which can act in a variety of ways: some reduce inflammation, others inhibit the generation of reactive oxygen species in the mitochondria, and others can improve mitochondria’s morphology. While these compounds have mainly been tested in cell or animal models of PD, future research may translate into clinical trials in humans.






