Mitochondria and the Many Disorders That Compose “Mitochondrial Disease”
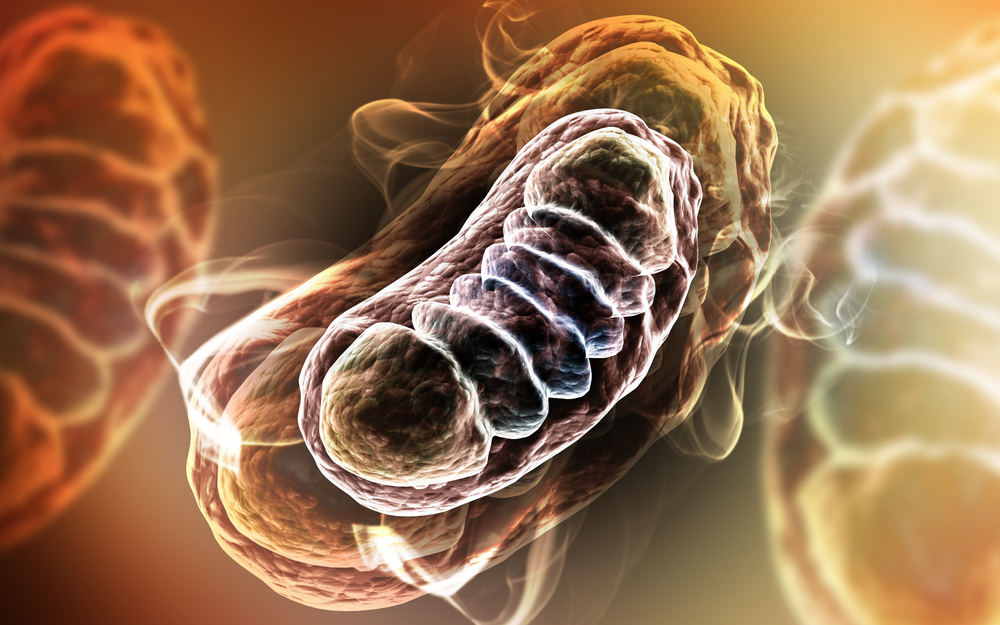
Mitochondria (singular mitochondrion) are tiny subunits present inside every cell of the human body except red blood cells, from the skin to the deep internal organs. Mitochondria’s main role is transforming food and oxygen that enter the cells into useful energy, creating more than 90 percent of the energy needed by the body to sustain life and support. The term “mitochondrion” derives from the Greek mitts (“thread”), and chondrion (“granule” or “grain-like”). More technically, mitochondria are double membrane-bound organelles — specialized subunits within cells with a specific function that are found in most eukaryotic cells (cells that have a nuclear envelope, cytoplasmic organelles, and a cytoskeleton).
Mitochondria are tiny, ranging from 0.5 to 1.0 micrometers in diameter, with considerable observable variations in the structure and size of the organelle, and are sometimes described as “the powerhouses of the cell” because they generate most of the cell’s supply of adenosine triphosphate (ATP), used as a source of chemical energy, and are involved in various other tasks, such as signaling, cellular differentiation, and cell death, as well as maintaining control of the cell cycle and cell growth.
However, the Pittsburgh, Pennsylvania-based United Mitochondrial Disease Foundation contends that regarding mitochondria primarily as energy-converters is an over-simplification that has slowed progress toward understanding the biology underlying mitochondrial disease. The UMDF notes that it takes about 3000 genes to make a mitochondrion, and mitochondrial DNA encodes just 37 of these genes, with the remaining preponderance of genes encoded in the cell nucleus and the resultant proteins transported to the mitochondria. Ergo: only about three percent of the genes necessary to make a mitochondrion (i.e.: 100 of 3000) are allocated for making ATP, while more than 95 percent (i.e.: 2900 of 3000) are involved with other functions tied to the specialized duties of the differentiated cell in which the mitochondrion resides, and these duties change as we develop from embryo to adult and as our tissues grow, mature, and adapt to the postnatal environment. It is these other non-ATP-related functions that are intimately involved with most of the major metabolic pathways used by a cell to build, break down, and recycle its molecular building blocks, and the cells themselves can’t even make the RNA and DNA they need to grow and function without the function of mitochondria. The building blocks of RNA and DNA are purines and pyrimidines, and it is the mitochondria that contain the rate-limiting enzymes for pyrimidine biosynthesis (dihydroorotate dehydrogenase) and heme synthesis (d-amino levulinic acid synthetase) required to make hemoglobin.
Similarly, liver cells’ mitochondria are specialized to detoxify ammonia in the urea cycle, and mitochondria are also required for cholesterol metabolism, estrogen and testosterone synthesis, neurotransmitter metabolism, and free radical production and detoxification, in addition to breaking down (oxidizing) the fat, protein, and carbohydrates we eat and drink.
Researchers at the National Institutes of Health report the first clear evidence that muscle cells distribute energy primarily by the rapid conduction of electrical charges through a vast, interconnected network of mitochondria in a way resembling the wire grid that distributes power throughout a city. The study, published the journal Nature, entitled: “Mitochondrial reticulum for cellular energy distribution in muscle“ (Nature 523, 617–620 (30 July 2015) dpi:10.1038/nature14614) provides an unprecedented, detailed window into showing how the system that rapidly distributes energy throughout the cell to power muscle contraction works. These observations solve the problem of how muscles rapidly distribute energy within the cells for movement.
Mitochondria have also been implicated in a number of human diseases, including a class of pathology known collectively as mitochondrial disorders as well as cardiac dysfunction and heart failure. Findings of a recent small University of California study suggest that autism may also be correlated with mitochondrial defects as well.
“Mitochondrial Disease” Includes Many Different Disorders
The term “Mitochondrial disease” refers to a broad range of disorders, each of which involves a mitochondrial dysfunction, with many more believed to have yet to be discovered. Because mitochondria perform so many different functions in different tissues, there are literally hundreds of different mitochondrial diseases that result from either inherited or spontaneous mutations in mtDNA or nDNA, which lead to altered functions of the proteins or RNA molecules that normally reside in mitochondria.
Another subcategory is Mitochondrial myopathies — a group of neuromuscular diseases caused by damage to the mitochondria — with some examples including Kearns-Sayre syndrome (KSS), Leigh’s syndrome, Mitochondrial Depletion syndrome (MDS), Mitochondrial Encephalomyopathy, Lactic Acidosis and Stroke-like episodes (MELAS), Myoclonic epilepsy with Ragged Red Fibers (MERRG), Mitochondrial neurogastrointestinal encephalopathy syndrome (MNGIE), Neuropathy, Ataxia, and Retinitis Pigmentosa (NARP), Pearson syndrome, and Chronic Progressive External Opthalmoplegia (CPEO). Nerve cells in the brain and muscles require a great deal of energy and appear to be particularly vulnerable when mitochondrial dysfunction occurs.
Each particular condition is the result of a genetic mutation — a specific change in the genetic material of the mitochondria — that causes the mitochondria to fail, which in turn leads to less and less energy getting converted in the cells, which may stop working or die. Depending on the location of the affected cells, certain parts and/or functions of the body may no longer function properly, leading to health problems and symptoms that can range from mild to severe. Because of the complex interaction between the hundreds of genes and cells that must cooperate to keep the body’s metabolic machinery running smoothly, it is a hallmark of mitochondrial diseases that identical mtDNA mutations may not produce identical diseases. Genocopies are diseases that are caused by the same mutation but may not look the same clinically, which complicates diagnosis.
Mitochondrial disease primarily affects children, but adult onset is becoming more and more common, and there is a broad spectrum of metabolic, inherited and acquired disorders in adults in which abnormal mitochondrial function has been postulated or demonstrated. It is estimated that at least one in 6000 people and as many as one in 4000 have a mitochondrial disease, with approximately 20,000 people in the United States believed to have a form of mitochondrial myopathy, for which there is currently no cure, and approximately 1,000 to 4,000 American children born with the disorder each year. If mitochondrial failure is repeated throughout the body, whole systems begin to fail, and the life of the person in whom this is happening is severely compromised. Diseases of the mitochondria that appear to cause the most damage are ones affecting cells of the brain, heart, liver, skeletal muscles, kidney and the endocrine and respiratory systems. On the other hand, many people affected can have normal life spans with their disease well managed, and research is underway across the world that will enhance knowledge regarding these diseases and discovery of new treatments and therapies.
Symptoms of mitochondrial disease may include diminishment or loss of motor control, muscle weakness and pain, gastrointestinal disorders, swallowing difficulties, poor growth, fatigue, lack of endurance, poor balance, cardiac disease, liver disease, diabetes, respiratory complications, seizures, visual/hearing problems, lactic acidosis, developmental delays, skeletal muscle abnormalities, and susceptibility to infections, nervous system impairment.
Symptoms of mitochondrial myopathies include muscle weakness or exercise intolerance, heart failure or rhythm disturbances, dementia, movement disorders, stroke-like episodes, deafness, blindness, droopy eyelids, limited mobility of the eyes, vomiting, and seizures.
Most mitochondrial myopathies occur before the age of 20, and often begin with exercise intolerance or muscle weakness. During physical activity, muscles may become easily fatigued or weak. Muscle cramping is rare, but may occur. Nausea, headache, and breathlessness are also associated with these disorders.
The National Institutes of Health (NIH) notes that while there is no specific treatment for any of the mitochondrial myopathies, physical therapy may extend the range of movement of muscles and improve dexterity, and vitamin therapies such as riboflavin, coenzyme Q, and carnitine (a specialized amino acid) may provide subjective improvement in fatigue and energy levels in some patients.
For information on NIH Patient Recruitment for Mitochondrial Myopathy Clinical Trials, see:
http://www.ninds.nih.gov/disorders/mitochondrial_myopathy/mitochondrial_myopathy.htm
Reata’s MOTOR Study For Treating Mitochondrial Myopathies
Irving, Texas based Reata Pharmaceuticals, Inc. a privately held company dedicated to translating innovative research into breakthrough medicines for difficult-to-treat diseases that have significant unmet needs, last month announced the enrollment of the first patient in MOTOR, a Phase 2 dose-ranging study examining the safety, tolerability, and efficacy of Reata’s drug candidate RTA 408 Oral Capsules for treatment of patients with mitochondrial myopathies (MM). MOTOR is a multi-center study planned for approximately 52 patients with MM.
The primary efficacy endpoint of the MOTOR study is the change in peak workload (Watts/kg) during exercise testing, and the secondary endpoint includes a patient’s 6-minute walk distance. The study is also exploring the change in peak oxygen utilization during maximal exercise testing and changes in the Fatigue Severity Scale.
“Emerging translational research demonstrates that activation of Nrf2 (the target of RTA 408) can improve mitochondrial function and cellular energy production. These observations underlie our hypothesis that RTA 408 may improve exercise capacity and quality of life in patients with mitochondrial myopathies,” says Dr. Colin Meyer, Reata’s Chief Medical Officer in a recent Reata press release. “We are hopeful that RTA 408 will benefit mitochondrial myopathy patients, and we appreciate the guidance and support that Reata has received from the UMDF and the MM patient community.”
 “We are very excited this trial will be underway with its first patient,” says Charles A. Mohan, Jr. , Executive Director and CEO of the United Mitochondrial Disease Foundation, in the same release. “Coordination, communication and collaboration between our industry partners and our patients to promote and support clinical trials is the only way we will accelerate the development of diagnostic tools, therapies, and potential cures for mitochondrial disease. We are pleased with the role Reata has taken in this endeavor and honored to call them a partner. We must all remember; no patients no trials, no trials no treatments nor cures.”
“We are very excited this trial will be underway with its first patient,” says Charles A. Mohan, Jr. , Executive Director and CEO of the United Mitochondrial Disease Foundation, in the same release. “Coordination, communication and collaboration between our industry partners and our patients to promote and support clinical trials is the only way we will accelerate the development of diagnostic tools, therapies, and potential cures for mitochondrial disease. We are pleased with the role Reata has taken in this endeavor and honored to call them a partner. We must all remember; no patients no trials, no trials no treatments nor cures.”
For more information on this study, visit:
https://clinicaltrial.gov/ct2/show/NCT02255422
RTA 408 and Bioenergetics Effect
According to Reata, RTA 408 activates the body’s anti-oxidative pathways through transcription factor Nrf2 and is able to improve mitochondrial function. In mouse models of bioenergetic disease, RTA 408 demonstrated the ability to increase glucose uptake, fatty acid oxidation and oxygen consumption, direct signs of healthier cellular metabolism (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3003357). RTA 408 analogs have also demonstrated in mouse models of oxidative stress the ability to induce genes related to mitochondrial biogenesis through the activation of Nrf2, which showed signs of potentially improving muscle function (http://www.ncbi.nlm.nih.gov/pubmed/21457778).
Stealth BioTherapeutics – Bendavia and Ocuvia
Another biopharmaceutical company developing drug candidates for treating mitochondrial disease is Stealth BioTherapeutics of Boston, Massachusetts, whose Chief Executive Officer Travis Wilson presented a corporate overview and development update on July 8 at Cantor Fitzgerald’s Inaugural Healthcare Conference in New York City.
Stealth’s lead candidates, Bendavia and Ocuvia, are investigational drugs with the potential to modify disease processes through mitoprotection — the ability to preserve energetics and restore normal energy production in mitochondria, while decreasing oxidative stress. These two clinical candidates are being developed for both common and rare diseases including inherited mitochondrial diseases, where there are no FDA-approved treatments.
The clinical development for Bendavia and Ocuvia has been structured to demonstrate patient benefit across multiple therapeutic areas during 2015 and continue toward later-stage trials and registration in both rare and common diseases.
Bendavia targets mitochondrial dysfunction, a key element believed to be at the root of a variety of serious, debilitating diseases, and has been developed to treat an underlying defect in mitochondria to reduce oxidative stress and increase energy supply to affected cells and organs. Bendavia penetrates the cellular and outer mitochondrial membranes, and targets cardiolipin, which is found exclusively in the inner mitochondrial membrane. Bendavia has been shown to positively impact dysfunctional mitochondria in nonclinical studies, with no effect in healthy mitochondria. In this way, Bendavia may address mitochondrial disease and dysfunction, where no FDA-approved treatments currently exist.
Ocuvia, a mitoprotective agent for retinal diseases, has in nonclinical studies demonstrated potential to be the first investigational topical ophthalmic formulation to treat back-of-eye diseases, offering a pragmatic alternative to treatments that require physician-administered ocular injections. Ocuvia is designed to treat the underlying defects in mitochondria associated with diseases such as Diabetic Macular Edema, genetic Mitochondrial Optic Neuropathies and Age-related Macular Degeneration. These defects include excessive oxidative stress and decreased energy supply to affected cells of the eye, particularly in the retina.
Stealth notes that the science underlying Bendavia and Ocuvia is supported by more than 100 independent, peer-reviewed publications and abstracts, and that these mitochondrial-targeted candidates represent a novel therapeutic approach to address a wide variety of diseases having unmet treatment needs including orphan mitochondrial diseases and mitochondrial medicine. More information about Stealth and its candidate pipeline can be found at: http://StealthBT.com
Raptor Pharmaceutical Corp. – PROCYSBI (Cysteamine Bitartrate)
 Novato, California based Raptor Pharmaceutical Corp. is another emerging global biopharmaceutical company focused on developing and commercializing therapeutics to treat rare diseases and unmet needs.
Novato, California based Raptor Pharmaceutical Corp. is another emerging global biopharmaceutical company focused on developing and commercializing therapeutics to treat rare diseases and unmet needs.
On Monday, August 17, Raptor announced that it has received U.S. Food and Drug Administration (FDA) approval for the expanded use of its drug RP103, currently marketed in the U.S. as PROCYSBI (cysteamine bitartrate), delayed-release capsules to treat children two to six years of age with nephropathic cystinosis. The company has active clinical development programs in multiple therapeutic areas such as nephropathic cystinosis, nonalcoholic fatty liver disease, Huntington’s disease (HD), and Leigh syndrome and other mitochondrial disease.
Despite their distinct clinical pictures, mitochondrial diseases share a common feature that mitochondria’s ability to produce energy is damaged and consequently the mitochondria is further damaged due to subsequent byproducts accumulation and interference with other chemical reactions in the cells.
Treatment of inherited mitochondrial diseases with cysteamine is potentially based on different mechanisms of action than that for treatment of cystinosis, although Raptor says one key biochemical reaction, which is the basis for the treatment of cystinosis, seems to play a significant role also. Cysteamine is an aminothiol that participates in a thiol-disulfide interchange reaction converting cystine into cysteine and cysteine-cysteamine mixed disulfide. This cysteine-cysteamine mixed disulfide can exit the lysosome through the lysosome membrane as it is transported through the intestinal barrier or the blood brain barrier, by the lysine transporter or a lysine-like transporter, the PQLC2 protein. This biochemical reaction results in an increase of the cellular thiol pool, making more cysteine available for glutathione (GSH) synthesis. Glutathione is composed of the amino acids cysteine, glutamate and glycine. Availability of cysteine, which exists primarily as cystine, is the major rate-limiting factor in GSH production.
Leigh syndrome is a severe neurological disorder caused by genetic defects in mitochondrial or nuclear DNA affecting respiratory chain function that typically results in death within the first decade of life. The condition causes increased production of reactive oxygen species which disrupts mitochondrial electron transport and affects cellular function in a variety of tissues. Typically observed during the first year of life, Leigh syndrome is characterized by a failure to thrive, lack of coordination, involuntary and sustained muscle contraction, muscle wasting, and multiple organ failure. The incidence of Leigh syndrome in the U.S. is estimated to be 1 in 40,000 newborns.
 “Leigh syndrome is one of the most devastating of mitochondrial disorders,” says Bruce H. Cohen, M.D. , Professor of Pediatrics and Director of Neurology at Akron Children’s Hospital, and lead investigator of an RP103 clinical trial in a Raptor release. “RP103 may stimulate steady and continuous depletion of reactive oxygen species which are toxic to cellular function and structure. These reactive oxygen species are abnormally high in patients with Leigh syndrome.” Dr. Cohen served on the board of trustees of the United Mitochondrial Disease Foundation from 1999 to 2006, was a member of the UMDF’s Scientific and Medical Advisory board, and was reappointed to the board of trustees in 2010.
“Leigh syndrome is one of the most devastating of mitochondrial disorders,” says Bruce H. Cohen, M.D. , Professor of Pediatrics and Director of Neurology at Akron Children’s Hospital, and lead investigator of an RP103 clinical trial in a Raptor release. “RP103 may stimulate steady and continuous depletion of reactive oxygen species which are toxic to cellular function and structure. These reactive oxygen species are abnormally high in patients with Leigh syndrome.” Dr. Cohen served on the board of trustees of the United Mitochondrial Disease Foundation from 1999 to 2006, was a member of the UMDF’s Scientific and Medical Advisory board, and was reappointed to the board of trustees in 2010.
In addition to providing an antioxidant activity directly, RP103 is believed to increase mitochondrial glutathione which acts as a scavenging agent of reactive oxygen species. Reactive oxygen species are a byproduct of mitochondrial energy production and place oxidative stress on cells. In patients with mitochondrial dysfunction, these reactive oxygen species are produced at dangerously high levels. By increasing levels of the antioxidant glutathione in the mitochondria, RP103 may reduce the toxic oxidative stress typically associated with mitochondrial disorders.
For more information, visit:
http://www.raptorpharma.com/
Sources
United Mitochondrial Disease Foundation
Reata Pharmaceuticals, Inc.
Stealth BioTherapeutics
Raptor Pharmaceutical Corp.
MitoCanada Foundation
National Institutes of Health
Nature






