Review on the Link Between Macrophages, Mitochondria and Inflammation in Atherosclerosis Development
Two researchers at Glasgow Caledonian University in the United Kingdom recently published a review focused on atherosclerosis and the role of mitochondria in the regulation of macrophages (a type of white blood cell) sterol metabolism and the inflammatory responses. The review was published in the World Journal of Cardiology and is entitled “Mitochondrial function and regulation of macrophage sterol metabolism and inflammatory responses.”
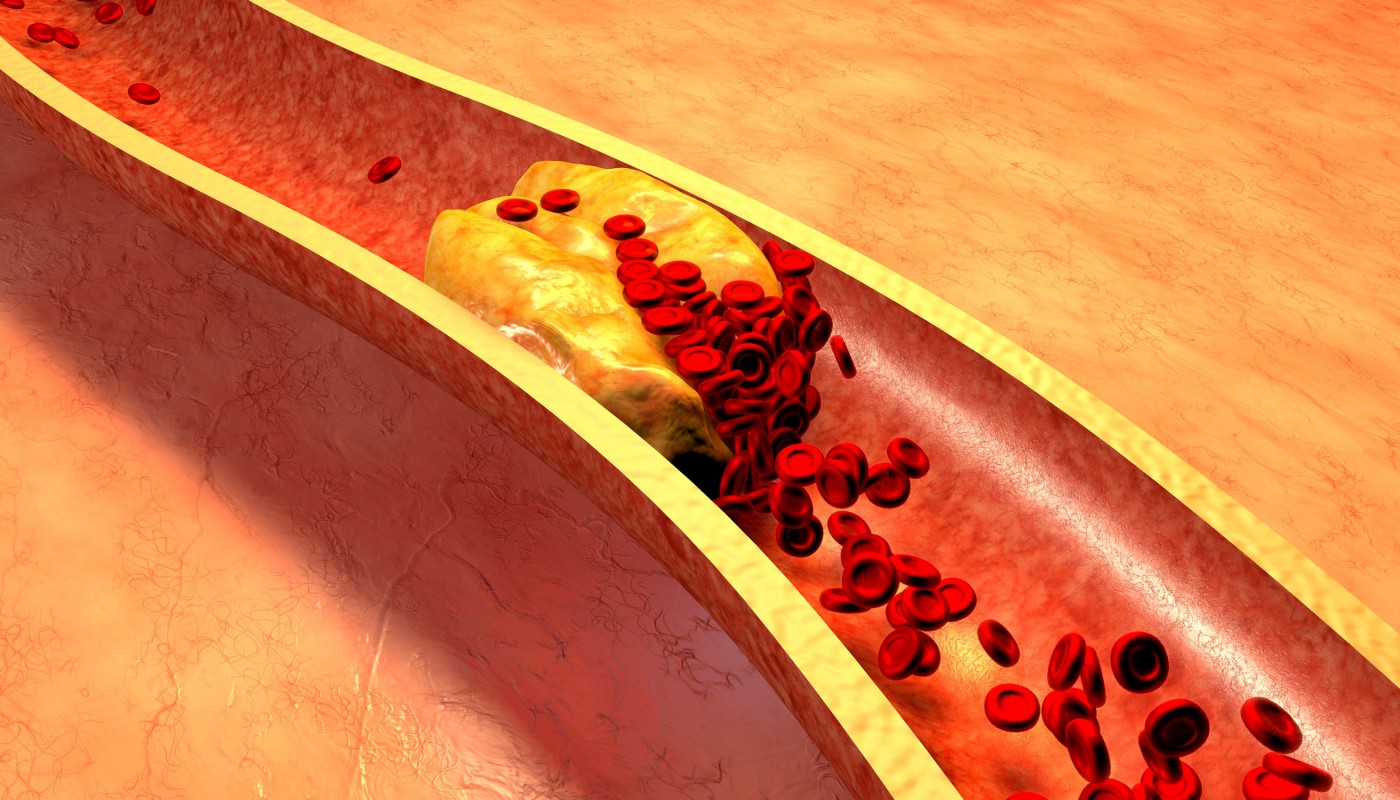
Atherosclerosis is a disorder in which plaques (composed of fat, cholesterol and calcium, among other substances) progressively accumulate inside the arteries. Over time, these plaques harden and obstruct the arteries, compromising the flow of oxygen-rich blood throughout the body. Atherosclerosis can lead to serious conditions such as heart attack (myocardial infarction), stroke (cerebrovascular accident) and even death.
Atherosclerosis is the primary cause of coronary heart disease, a disorder in which plaques accumulate inside the coronary arteries that supply oxygen-rich blood to the heart muscle. Coronary heart disease is a major cause of morbidity and mortality worldwide.
[adrotate group=”4″]
Increased levels of low density lipoprotein (LDL) lead to their accumulation within the arterial wall, ultimately triggering the recruitment of white blood cells. These white blood cells (mostly macrophages), in what is thought to be a protective mechanism, uptake the excess cholesterol; however, macrophages can become overloaded with cholesterol, accumulate in the atherosclerosis lesions sites (a process called “fatty streaks”) and induce a chronic, unresolved inflammatory response, accelerating disease progression.
Cholesterol trafficking within the macrophage is performed through mitochondria, cellular organelles known to play a crucial role in the immune system, especially in regulating the responses of macrophages to tissue injury and inflammation. Mitochondrial dysfunction has been linked to the inflammatory vascular reaction that leads to atherosclerosis lesions and to coronary syndromes.
According to the study authors, removal of the cholesterol from macrophages may ultimately protect against coronary heart disease. High density lipoprotein (HDL) particles, for instance, can counteract the chronic inflammation seen in atherosclerosis. It is known that a part of the HDL beneficial effects are due to the interaction of ATP binding cassette (ABC) transporters (ABCA1, ABCG1 and ABCG4) with apolipoproteins and HDL, which leads to the removal of cholesterol and limits the production of inflammatory cytokines. However, increasing the HDL levels does not necessarily guarantee protection against coronary heart disease.
The authors concluded that the mitochondrial cholesterol trafficking in macrophages and the production of inflammatory cytokines are linked to atherosclerosis. The team suggests that therapeutic strategies aiming at an improvement in mitochondrial function may limit or induce a regression in atherosclerosis development and consequently reduce the incidence of coronary heart disease.






