Stem Cell Transplant Studied in MNGIE
A currently-recruiting Phase 1 clinical trial will identify if stem cell transplants are a safe treatment option for the rare disease mitochondrial neurogastrointestinal encephalopathy syndrome (MNGIE). The study aims to recruit 12 patients with MNGIE and treat them with allogeneic hematopoetic stem cells collected from the bone marrow or blood of donors.
To understand the reasoning behind allogeneic hematopoetic stem cell transplantation (AHSCT) for MNGIE, the molecular reason for MNGIE must first be understood. The disease occurs as a result of two inherited DNA mutations in the gene encoding for the enzyme thymidine phosphorylase (TP). The mutation results in low or no TP activity, affecting storage of thymidine and deoxyuridine in mitochondria of cells. Toxic accumulations of thymidine and deoxyuridine affect energy production in the mitochondria, resulting in the symptoms of MNGIE.
The authors of the trial, “MNGIE AHSCT Safety Study (MASS),” believe AHSCT will replace TP enzyme in MNGIE patients and improve symptoms due to better metabolism of thymidine and deoxyuridine. Although the collaborators on the trial have researched and designed an optimal AHSCT treatment plan, the safety of this treatment has not yet been tested.
[adrotate group=”4″]
“In this study, we plan to perform AHSCT on at least 3 and at most 12 patients with confirmed MNGIE,” wrote Dr. Michio Hirano of Columbia University. “We will evaluate mortality, the success of the transplant, biochemical parameters, gastrointestinal function, and nerve functions. If the study shows that AHSCT for MNGIE is sufficiently safe, we plan to follow it with another study comparing AHSCT to standard of care (SOC) in MNGIE.” Primary outcome measures include the occurrence of primary graft failure within 42 days of transplantation and mortality within 100 days of transplantation.
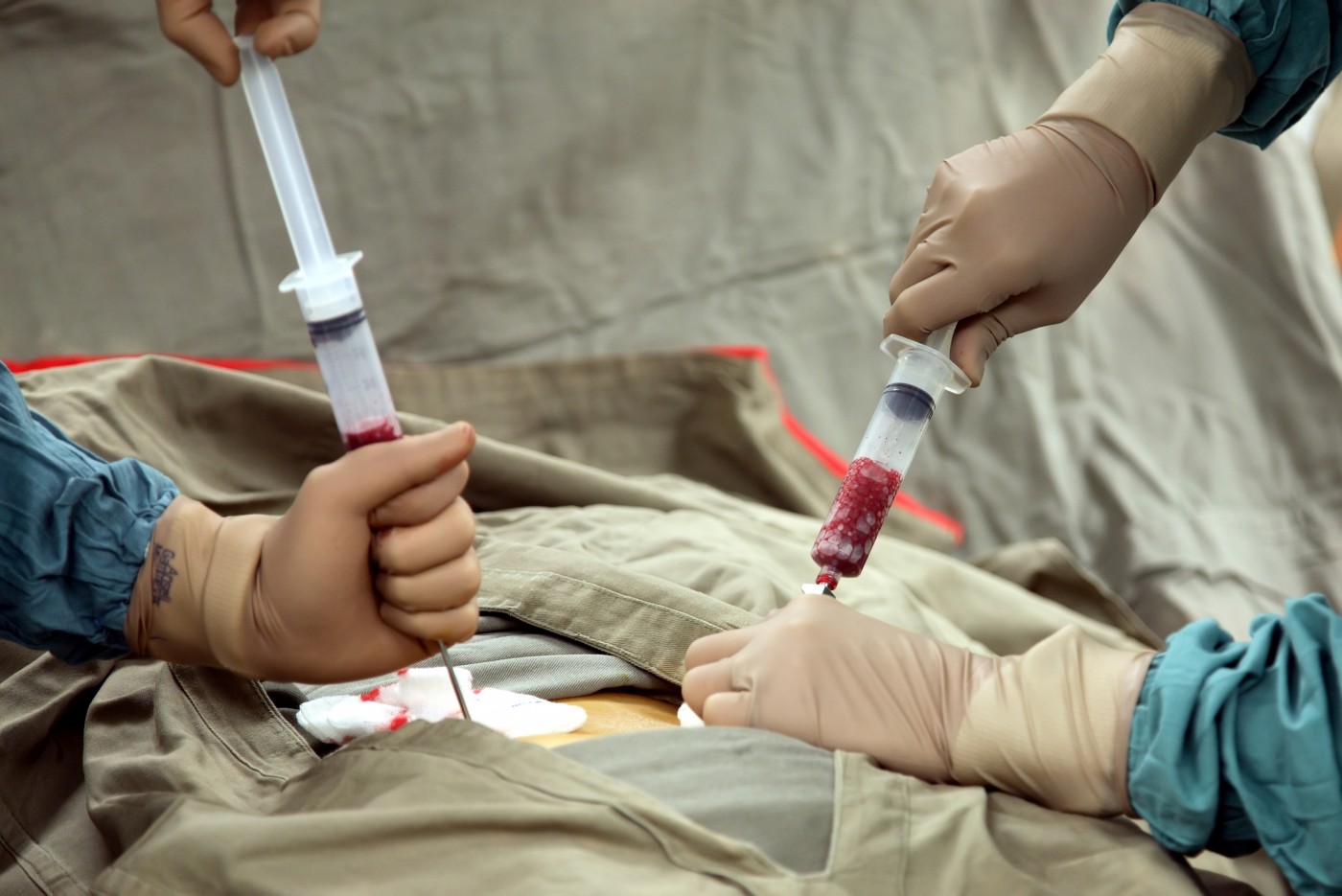
Allogeneic hematopoetic stem cells will be obtained from donors’ bone marrow or from peripheral blood after stimulation wit granulocyte colony-stimulating factor (G-CSF). Donors may be related or unrelated to recipients.
The clinical trial is sponsored by Dr. Hirano in collaboration with Rare Diseases Clinical Research Network, National Institutes of Health, National Institute of Neurological Disorders and Stroke, Eunice Kennedy Shriver National Institutes of Child Health and Human Development, Office of Dietary Supplements, and Weill Medical College of Cornell University. The trial was initiated after preliminary studies of AHSCT in other rare metabolic diseases such as Hurler syndrome, where patients lack alpha-L-iduronidase and cannot break down long sugar molecules (glycosaminoglycans). Other diseases have shown improvements following AHSCT, potentially due to a replacement of deficient enzymes. Since preliminary studies showed that transient platelet transfusions are sufficient to decrease thymidine levels for two to three days, the researchers believe permanent TP replacement via AHSCT will benefit patients with MNGIE.






