Peptide-Mediated Mitochondrial Delivery for MERRF Treatment Outlined in New Study
If myoclonic epilepsy with ragged red fibers (MERRF) syndrome is caused by at least one of four point mutations in mitochondrial DNA, then curing the disease should be as easy as giving new mitochondria to patients. However, this is a theoretical treatment easier said then done because delivering mitochondria to deficient cells within the human body is a difficult task. One group of researchers is investigating how cell-penetrating peptides can be used to deliver mitochondria to MERRF patient-derived human cells, and they have so far been successful in their approach.
“The present study further illustrates the feasibility of mitochondrial intervention therapy using the novel approach of peptide-mediated mitochondrial delivery and the benefit resulting from mitochondria-organelle manipulation,” wrote Dr. Jui-Chih Chang, lead author of the article “Treatment of Human Cells Derived from MERRF Syndrome by Peptide-Mediated Mitochondrial Delivery,” which was published in the journal Cytotherapy.
[adrotate group=”4″]
This study is one step of many to determine the feasibility of treating MERRF with mitochondrial transfer. Mitochondrial transfer, also referred to as mito-transfer, is an approach that addresses reduced endogenous mitochondrial function by delivering exogenous mitochondria. In theory, the treatment is enabled by rapid mitochondrial fusion and division and works to maintain homeostasis in cells. In practice, delivering mitochondria to cells requires a system that can penetrate the cell membrane and release the mitochondria inside the cell.
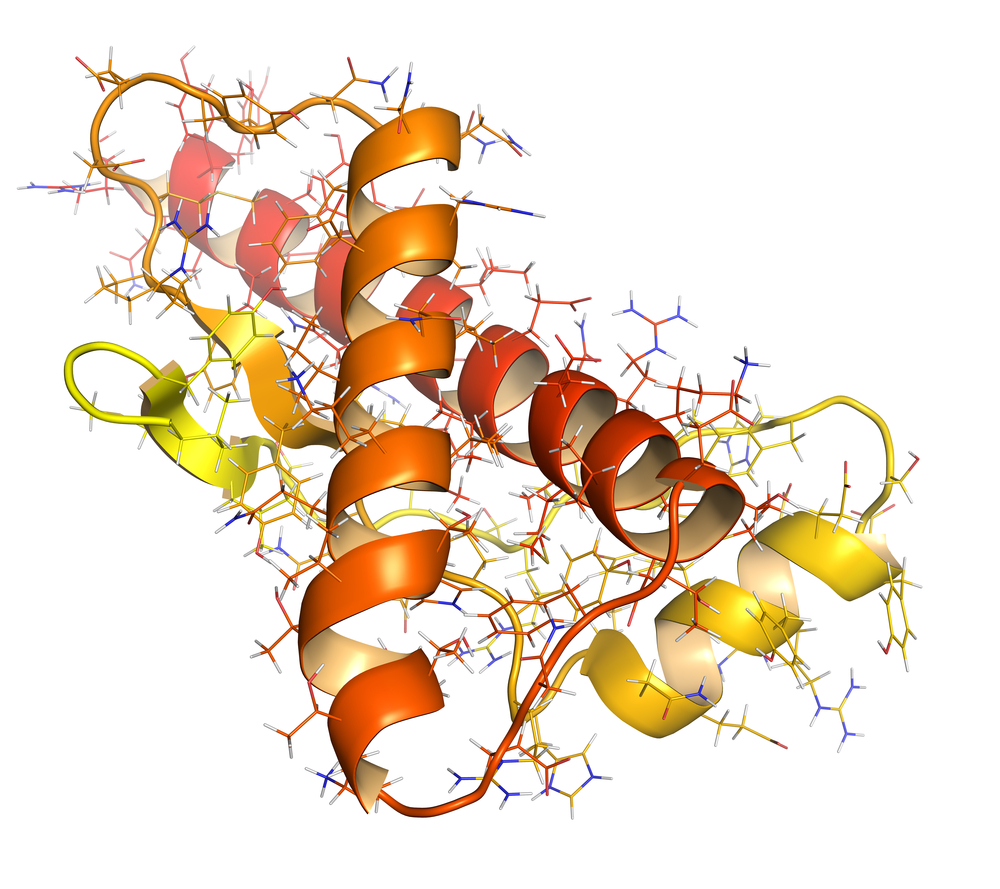
To address this need, Dr. Chang and the rest of his research team at Changhua Christian Hospital in Taiwan isolated mitochondria from healthy females’ and female MERRF syndrome patients’ dermal fibroblasts. The MERRF-derived cells had greater than 85% mutation in the tRNALys mitochondrial DNA, which is one of the four MERRF-associated mutations that is also associated with severe disease symptoms. After, the team attached a special peptide, named Pep-1, to the mitochondria. Pep-1 contains three regions, each with a unique purpose. The three domains (hydrophobic tryptophan-rich motif, hydrophilic lysine-rich domain, and spacer domain) work together to penetrate the cell membrane of cells without altering the cell membrane or harming cells.
“Isolated [mitochondria] were delivered into the MERRF fibroblasts at doses of 52.5 μg, 105 μg and 210 μg after Pep-1 conjugation,” wrote Dr. Chang. “After 21 days of delivery, significant mitochondrial elongation was observed in the rescued MERRF fibroblasts treated with 105 μg (1.9-fold) and 210 μg Pep-1-Mito compared with the cells before treatment.” These morphologcial changes were accompanied by decreases in reactive oxygen species (ROS), which are usually elevated in MERRF due to deficient working mitochondria.
Although the study was conducted only with cells in in vitro cell culture, it provides an important step forward in developing treatments for MERRF. “The present results clearly confirmed again and supply more evidence to prove the viability of peptide-mediated mitochondrial delivery (PMD) as a therapy for MEERF syndrome through interventional manipulation of mitochondrial function in host cells,” wrote Dr. Chang. “PMD technology allows for the validation of in vitro cell-based models useful for understanding the molecular regulation of neurodegenerative disorders to provide insight into further strategies for therapeutic intervention in mitochondria-related disease.”






