Study into Mitochondrial Replacement Therapy Appears to Answer Key Question of DNA Compatibility
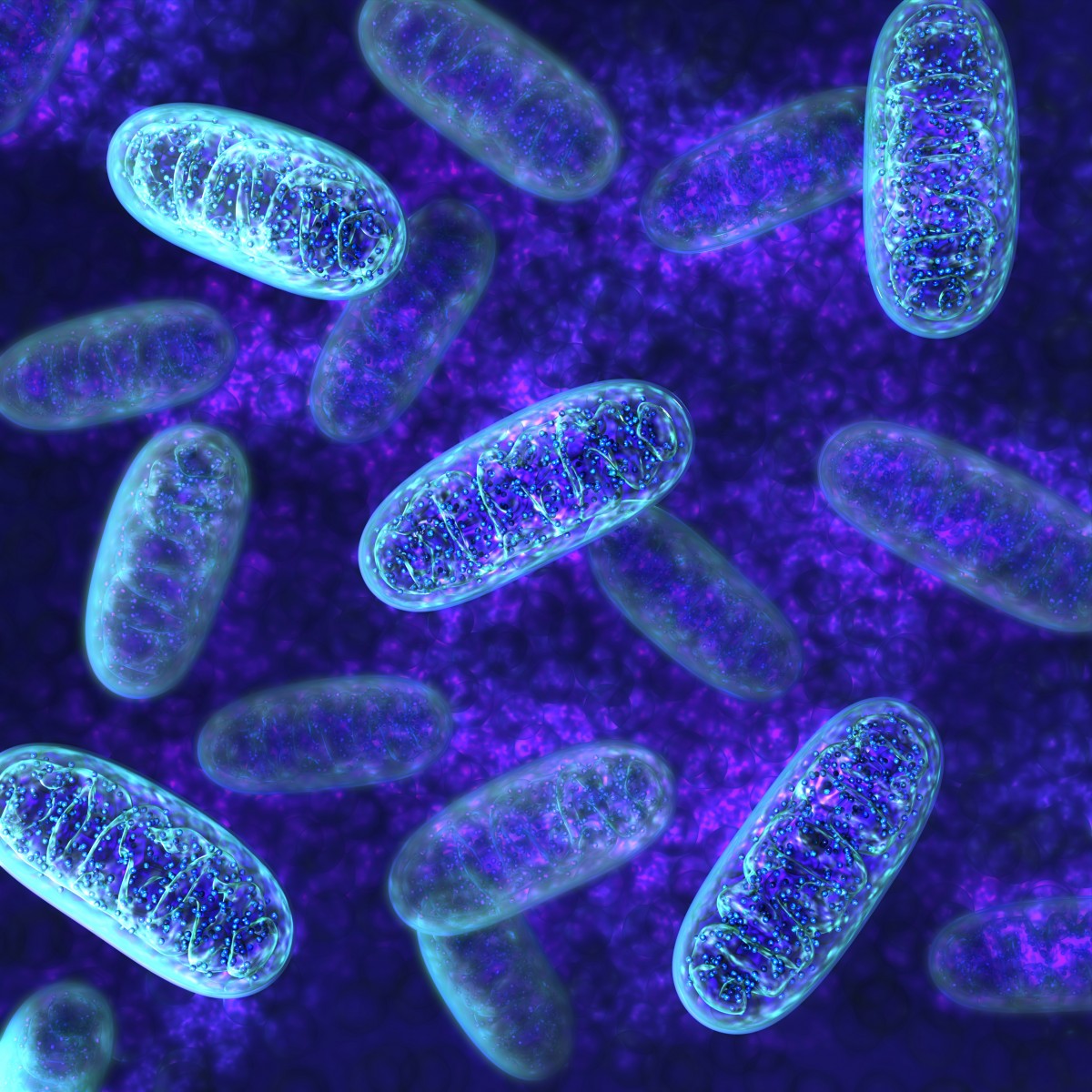
Mitochondrial replacement techniques may have taken a major step closer to clinical reality with a key study by the institute that invented the method — The New York Stem Cell Foundation (NYSCF) Research Institute. The findings demonstrated the compatibility of mitochondrial and nuclear DNA taken from two unrelated individuals, and underscored the necessity of not leaving any mutated mitochondria behind, since they can multiply through cell division and cause disease.
The study, “Genetic Drift Can Compromise Mitochondrial Replacement by Nuclear Transfer in Human Oocytes,” was published in the journal Cell Stem Cell.
Mitochondrial replacement is a source of hope for women carrying disease-causing mitochondrial mutations. While the method will not help patients living with mitochondrial disease, it could prevent the passing on of these mutations from a mother to her child if it reaches clinical practice.
In contrast to nuclear DNA, the mitochondrial DNA counterpart is inherited only from the mother, and women with malfunctioning mitochondria pass it along. In 2012, the NYSCF suggested that mitochondrial replacement techniques could break this chain, but important questions need to be answered before the method might be tested in humans. Research in mice has shown that when mitochondrial genomes from two mothers are experimentally combined, the mitochondrial DNA becomes unstable.
Scientists have also suggested that co-inheritance of nuclear and mitochondrial genomes is necessary for stability, and that replacing the mitochondria in an egg cell could cause dysfunction in the mitochondrial energy-producing complex, which is encoded by both nuclear and mitochondrial genes.
A mitochondrial transfer process is designed to replace diseased mitochondria in an egg cell with those from a healthy donor before the egg is fertilized in the lab, much as would take place in normal in vitro fertilization. Because of the earlier research showing mitochondrial DNA instability, however, researchers questioned whether combining nuclear and mitochondrial DNA from two unrelated donors was even possible.
Led by Dr. Dieter Egli, a senior research fellow at the NYSCF Research Institute and an assistant professor at Columbia University College of Physicians and Surgeons, the scientists found that nuclear and mitochondrial genomes are indeed compatible, even when they come from different people.
“This is one more step towards the therapeutic application of mitochondrial replacement and informs us how MRT [mitochondrial replacement therapy] is best conducted clinically,” Dr. Egli said in a press release.
Researchers also found that during mitochondrial transfer, a minute amount of mutated mitochondria might remain in the cell. Because of instability processes, these few mitochondria can follow two paths — either their numbers decrease and they become difficult to even detect, or, in rare cases, they start multiplying as cells divide, eventually reaching numbers counteracting the replacement.
“In order to prevent the transmission of mitochondrial diseases, we need to avoid competitive situations between mitochondrial genotypes of the parent and of the mitochondrial donor. The co-existence of the two-mitochondrial types within one cell must be avoided through minimizing or even eliminating carry-over during transfer,” said Dr. Egli.
“For women who are affected with these diseases, this work brings hope that they will have access to therapies that will allow them to have healthy children. Since our initial work with MRT, we have advocated for the FDA to permit clinical trials that enable women to prevent their children from inheriting mitochondrial diseases,” said Susan L. Solomon, co-founder and CEO of the NYSCF. “I hope this research provides further evidence to the FDA to approve this work for clinical application.”






