Scientists Develop New Peptides as Novel Therapies for Mitochondrial Diseases
A study led by researchers at Washington University School of Medicine and Albert Einstein College of Medicine found a new route to correct dysfunctional mitochondria. The scientists designed small compounds that could help treat Charcot-Marie-Tooth disease (CTMD) and other mitochondrial diseases.
The study, “Correcting mitochondrial fusion by manipulating mitofusin conformations,” was recently published in Nature.
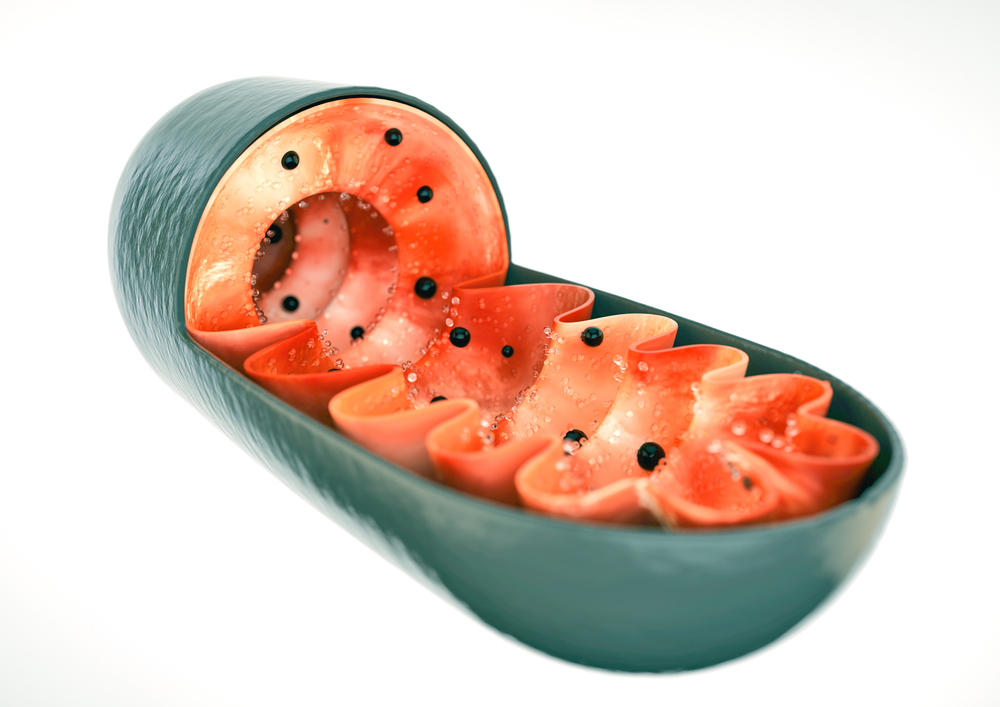
Mitochondrial disease is caused by dysfunctional mitochondria, the cell unit that converts the energy of food molecules into power that allows most cells to function properly. Mitochondrial disease affects almost 3 million people worldwide. The disease is characterized by progressive loss of motor neurons and leads to paralysis.
Most mitochondrial diseases, including CMTD, are currently incurable and treatment options are limited. Most treatments are designed to decelerate the progression of the disease.
In this study, researchers prepared novel molecules able to correct mitochondrial dysfunction. Testing the molecules on mouse models provided new insights about the structure and function of the disabled protein responsible for the dysfunction of mitochondria.
“This mitochondrial protein has never been targeted before,” senior author Gerald W. Dorn II, MD, the Philip and Sima K. Needleman Professor of Medicine, said in the press release.
“There are no drugs that work on this protein that is so important for mitochondrial function. We designed two compounds — one that activates and one that inhibits the function of this protein. We are working on testing them in mice with mitochondrial defects.”
The researchers examined the mitochondrial protein mitofusin 2, involved not only in CMTD but in many other diseases like diabetes and heart disease.
They found that folding and fusion between two mitochondria is controlled by mitofusin 2, which allows both units to exchange genetic information that plays a role in healthy function of mitochondria.
“In the past, scientists assumed mitofusin 2 was always active, always ready to tether to another mitofusin molecule and promote mitochondrial fusion,” Dorn said. “Our study now shows this is incorrect. Mitofusin 2 folds and unfolds, giving it active and inactive forms that either encourage or discourage tethering and the resulting fusion of mitochondria.”
The researchers synthetized tiny peptides that can activate or deactivate the mitofusin 2 protein. A small peptide dubbed GoFuse was found to activate mitofusin 2 and induce mitochondrial fusion. By contrast, a peptide dubbed TetherX inactivates mitofusin 2 and prevents mitochondrial fusion.
“We designed these molecules based on our new knowledge of mitofusin 2,” Dorn said. “My colleague, Dr. [Daria] Mochly-Rosen, is a genius at designing this kind of small peptide drug. She looks at amino acid sequences and sees things I don’t see.”
Mochly-Rosen said that designing the peptide inhibitors was challenging.
“But it is always exciting when a basic research discovery leads to the design of a new drug that may eventually help patients who currently have no treatment options,” she said.
The researchers believe these small peptides that activate and deactivate mitofusin 2 protein are promising new routes to pursue future searches for novel therapeutic agents for mitochondrial diseases and for decreasing tissue damage after a heart attack or stroke.






