Reduced Cellular Energy Leads to Cell Dysfunction in Neurodegenerative Diseases
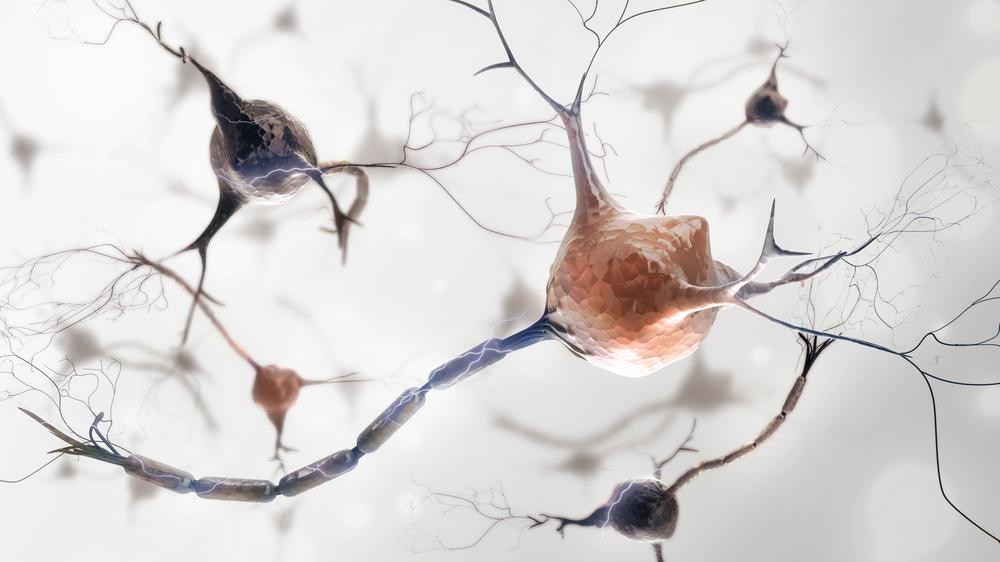
A recently published study by a team of researchers at the Gladstone Institutes, titled “The Role of Mitochondrially Derived ATP in Synaptic Vesicle Recycling“, is the first piece of evidence detailing how abnormalities in cell mitochondria can significantly reduce cellular energy and lead to dysfunctional brain cells. This was observed in models of neurodegenerative diseases. While the role of reduced cellular energy in neurodegeneration has long since been a subject of research, this study, authored by Gladstone Institute of Neurological Disease postdoctoral fellow Divya Pathak, Ph.D., is the first to create and successfully utilize a novel assay to quantify brain cell ATP (the energy molecule). The study is currently published and was selected as Paper of the Week in the Journal of Biological Chemistry.
Through a model of Leigh’s disease, a neurometabolic condition that affects cellular mitochondria, the researchers were able to use novel assays to examine cellular energy levels. They found that the cells in this disease, because it compromised mitochondrial output, were notably dysfunctional.
“It was always assumed that defects in mitochondria would result in a depletion of energy levels, which would be toxic to neurons,” said Dr. Pathak in a news release. “But no one had been able to prove this because the necessary assays were not available. Now that we’ve demonstrated the link between impaired mitochondria, a loss of ATP, and neuronal dysfunction, the next step is to see if this connection holds true in conditions like Parkinson’s disease and Alzheimer’s disease.”
Researchers were also successful in determining a cellular energy threshold, which is the minimum amount of energy a cell would need to conduct synaptic vesicle cycling – a process that allows neurotransmitters to function in the brain. They did this by inhibiting glycolysis, in effect forcing the cells to rely only on ATP from mitochondria and yielding more accurate, isolated results across the cycle. They found that cells needed higher amounts of energy during re-uptake of vesicles after the release of neurotransmitters.
The team also compared energy levels in boutons – the docks where neurotransmitters are released – in cells with and without mitochondria present. Interestingly, there was no significant difference in their energy levels, however this led the researchers to believe that under normal conditions, cell energy can shift rapidly from boutons with mitochondria to boutons without them. Further research would be needed to determine if boutons without mitochondria will exhibit dysfunction.
Senior author Ken Nakamura, MD, PhD, an assistant investigator at the Gladstone Institute of Neurological Disease, believes that carrying out these studies in both healthy and diseased cells is vital for interpreting the findings. “We really need to understand the basics of cell biology in a normal setting in order to comprehend changes in disease,” he explained. “It’s worth taking the time to study these underlying biological processes so that we can identify the best therapeutic targets for neurodegenerative disorders.”






